Labs 10A & 11A: The Cranial Nerves
Learning Objectives
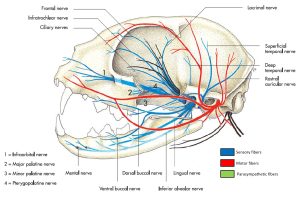
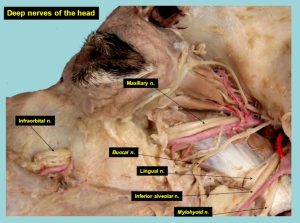
- Identify deep branches of the mandibular branch of the trigeminal n.
- Identify the superficial nerves of the lateral head and name their functions.
- Identify the important muscles of facial expression and known their innervation.
- Name and identify (or describe) CN I-XII, and identify their major branches.
- Identify the extraocular muscles and know their innervation.
- List each of the listed regular sensory, special sensory, somatic motor, and autonomic motor functions of cranial nerves I-XII.
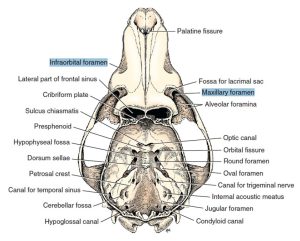
- Identify the major foramina in the skull through which the cranial nerves exit.
- Identify the relevant nerves for the different types of dental nerve blocks and where they pass through the bones of the skull.
Lab Instructions:
Dissect: In order to efficiently get through the dissection of the nerves of the head in a timely manner, we’ve bisected the heads into a left and right half. The dissection for each half will need to be performed concurrently. We’ll refer to a superficial and a deep dissection, which are to be carried out simultaneously. How to decide which half of the head will be used for which dissection? There are two options that we’ll present to you here, but you are encouraged to find your own solution if you find something more amenable to your group.
OPTION 1: Two members of the team can perform the superficial dissection while the other two team members work on the deep dissection of the head (the reader can split the ipad screen to facilitate this approach or a personal device or printed copy may be used). Obviously, both teams will need to round with the other team to go over the necessary material.
OPTION 2: Two superficial dissections are performed by the group simultaneously (two team members on each half). Then, one half is preserved for continued study of the superficial structures while the other is used by all four team members to then perform the deep dissection.
Make sure to review all of the structures on each side with your full team. Note that dissection points will be awarded as a team, so work together to ensure all steps are taken on both sides of the head.
Choosing sides for each dissection: During head bisection, if the larynx ended up more on one side, use that half for the deep dissection.
At the end of each dissection period, please wrap the head in a moistened paper towel and place it in a plastic bag.
- Cat superficial dissection
- Dog deep dissection
Got that sorted? Great, now let’s get into the dissection! For both the superficial and deep dissections, we’ll go through all twelve cranial nerves in order, specifically noting which ones are visible or accessible.
Superficial dissection
Start here if you are performing the superficial dissection.
Dissect: Carefully skin one half of your cadaver’s head and do your best to ensure that the superficial muscles, nerves, vessels, and ducts of the face (of which there are many) remain intact. Look at pro-sections to visualize how deep the plane of dissection should be. Leave a narrow rim of skin around the margin of the eyelids and at the edge of the lips. Preserve the nose and the philtrum, which is the median groove separating the right and left parts of the nose and superior lips. You need only skin to the base of the ear. A thin muscle known as platysma covers the majority of the structures of the face superficially. Sometimes this muscles comes away with the skin; if it remains, reflect platysma rostrally starting with its caudal edge. Take care to protect underlying nerves or vessels.
*A note regarding the superficial dissection: We’ll cover the majority of the relevant bony foramina here in this section. To identify these, grab a canine skull around the lab and some pipe cleaner to mimic a cranial nerve passing through. Also, make a point of showing your colleagues working on the deep dissection these bony foramina!*
Cranial Nerve I: The Olfactory Nerve
The olfactory nerve (CN I) consists of numerous axons that arise in the olfactory epithelium of the caudal nasal mucosa and pass through the foramina of the cribriform plate to the olfactory bulbs. These include axons from the vomeronasal organ that course along the nasal septum. No dissection is necessary.
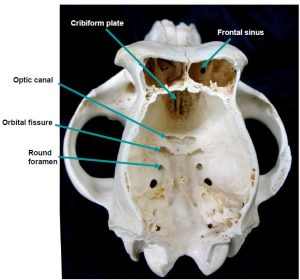
Observe: On a skull, identify the cribriform plate from inside the cranium. Looking at the medial surface of the bisected head, note the olfactory bulb sitting the most rostral part of the neurocranium, just dorsal to the cribriform plate.
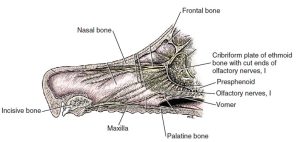
- Sagittal section of the nose to show distribution of nerves 3
Cranial Nerve II: The Optic Nerve
The optic nerve (CN II) is also referred to as the “prechiasmatic optic tract”. It is surrounded by the retractor bulbi muscle within the periorbita as it enters the caudal aspect of the bulbus oculi (eyeball). It is responsible for the special sense of vision. The optic nerves pass through the optic canals near the rostral end of the floor of the cranium.
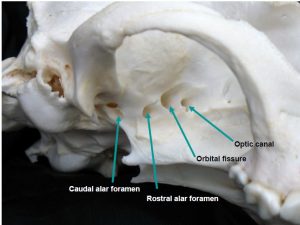
Observe: On a skull, identify the optic canal. This foramen can be found on the caudomedial aspect of the zygomatic arch, just dorsal to the pterygopalatine fossa. We will not dissect the optic n. in the superficial dissection.
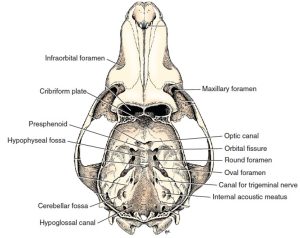
- Dog skull with foramina 1
Cranial Nerve III: The Oculomotor Nerve
The oculomotor nerve (CN III) passes through the orbital fissure and enters the periorbita with the optic n.
Observe: On a skull, identify the large orbital fissure just caudal to the optic canal. Cranial nerves III, IV, V1 (the ophthalmic n.), and VI all pass through the orbital fissure.
Once again, we will not dissect the oculomotor n. in the superficial dissection, and we will save the description of its associated structures and innervations for the deep dissection section.
- Dog skull with foramina 1
Cranial Nerve IV: The Trochlear Nerve
The trochlear nerve (CN IV) also passes through the orbital fissure and enters the periorbita. It innervates the dorsal oblique m. and need not be dissected.
Cranial Nerve V: The Trigeminal Nerve
The trigeminal nerve (CN V) divides into three nerves as it emerges from the trigeminal canal in the petrosal part of the temporal bone: the ophthalmic (V1), the maxillary (V2), and the mandibular (V3) nerves. We’ll discuss each of these in turn.
Ophthalmic n. (V1)
The ophthalmic n. passes through the orbital fissure and supplies sensory nerves that enter the periorbita. The ophthalmic n. and its branches need not be dissected. The frontal and infratrochlear nerves pass rostrally between the dorsal oblique and dorsal rectus muscles to innervate the medial aspect of the superior and inferior eyelids. Long ciliary nerves follow the optic nerve and innervate the eyeball. The ethmoidal nerve passes through an ethmoidal foramen and the cribriform plate to innervate the nasal mucosa and skin of the nose.
Maxillary n. (V2)
The maxillary n. passes through the round foramen and, in the dog enters the alar canal, exiting via the rostral alar foramen (in the cat, with no alar canal, it simply exits the round foramen). Its primary branches will be dissected in the deep half of the head.
Observe: On a skull, identify the round foramen. Note that in a dog skull, the ventral side of the round foramen enters the alar canal, and after passing through round foramen the maxillary n. exits this canal via the rostral alar foramen.
- Dog skull with foramina 1
Mandibular n. (V3)
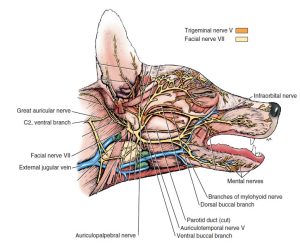
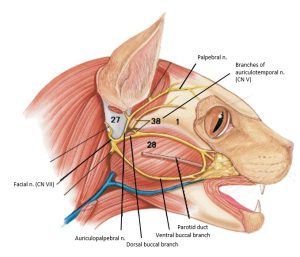
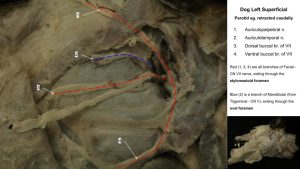
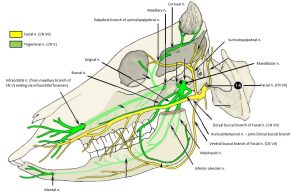
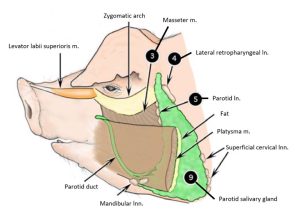
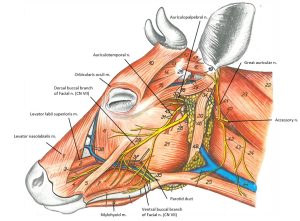
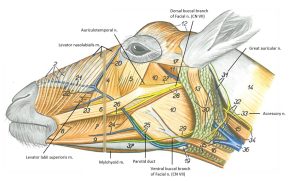
The mandibular n. exits the neurocranium via the oval foramen. A branch of the mandibular n., known as the auriculotemporal nerve, is apparent on the superficial dissection, lateral to the masseter m. The auriculotemporal nerve emerges just rostral to the facial nerve, between the caudal border of the masseter muscle and the base of the external acoustic meatus below the zygomatic arch. It may be found deep to the origin of the auriculopalpebral nerve.
On the superficial surface of the head, branches of the trigeminal nerve (CN V), including the auriculotemporal n., supply sensory innervation to the skin of the external ear (except inside surface of pinna) and the temporal, zygomatic, and masseteric regions. Branches of CN V, and more specifically the mandibular n., also provide motor innervation to the muscles of mastication.
Dissect: Isolate the auriculotemporal n. Importantly, its origin is from deep to the masseter muscle (the large muscle on the cheek, just ventral to the zygomatic arch), immediately rostral to the ear canal. This different relationship with the ear canal helps us distinguish the auriculotemporal n. from facial nerve branches (which are coming from caudal to the ear canal) when dissecting in the area deep to the parotid salivary gland.
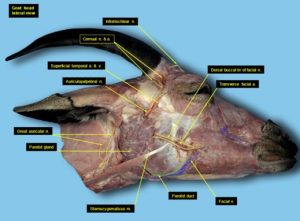
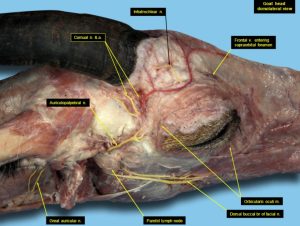
You may find it necessary to reflect the rostral edge of the parotid salivary gland (see images below to identify) to better visualize the auriculotemporal n.
The auriculotemporal n. provides sensory innervation that is generally described as the area extending dorsal and ventral from the zygomatic arch and caudal to the orbit. It also provides sensory innervation to the tympanic membrane and the skin lining the external acoustic meatus.
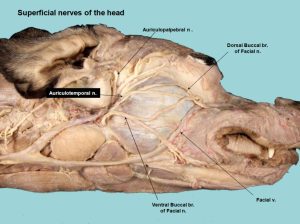
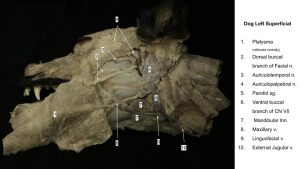
- Superficial branches of the facial and trigeminal nerves of the dog, lateral aspect. 1
- Superficial branches of the facial and ttigeminal nerves of the cat. 4
- Platysma remaining, reflected rostrally
Cranial Nerve VI: The Abducent Nerve
The abducent nerve (CN VI) passes through the orbital fissure and enters the periorbita. It innervates the retractor bulbi and the lateral rectus mm. We’ll dissect this nerve in the deep half of the head.
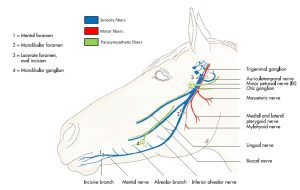
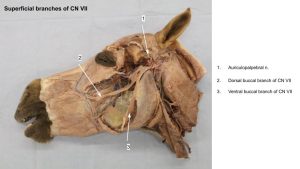
Cranial Nerve VII: The Facial Nerve
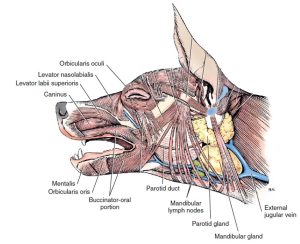
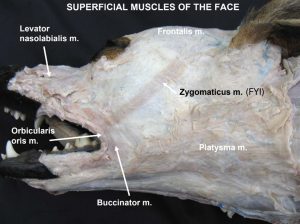
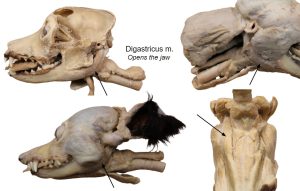
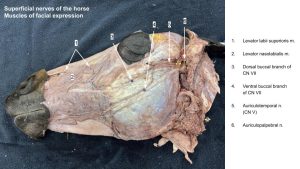
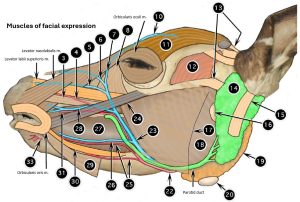
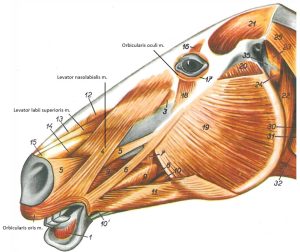
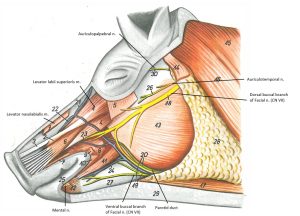
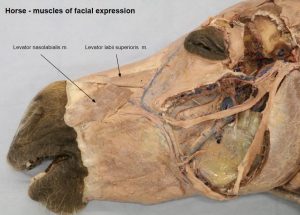
The facial nerve (CN VII) innervates all of the superficial muscles of facial expression (including: oribularis oris, buccinator, orbicularis oculi, and levator nasolabialis), the caudal belly of the digastricus muscle, and the platysma m. of the neck. The nerve enters the petrosal part of the temporal bone through the internal acoustic meatus, courses through the facial canal of that bone, and leaves the skull at the stylomastoid foramen just caudal to the external acoustic meatus, where it divides into several branches. As a general rule, on the superficial head, the facial nerve supplies motor innervation to the muscles of facial expression (exception: it also provides sensory to the inner surface of the pinna).
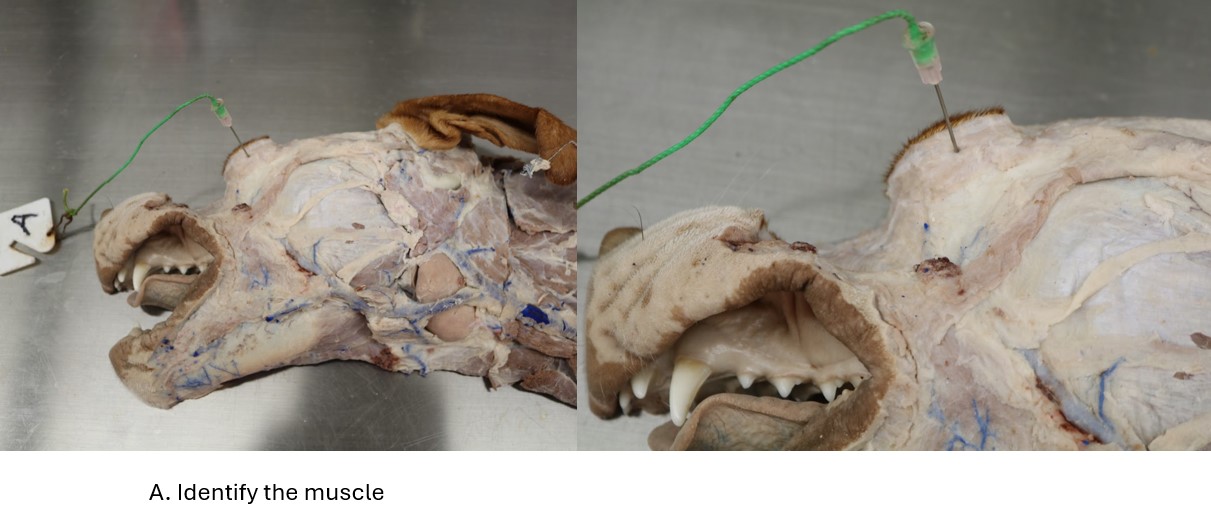
Observe: Before proceeding, identify the following muscles: digastricus m., platysma, orbicularis oris, buccinator, orbicularis oculi, and levator nasolabialis. Note that a portion of each of these muscles is often reflected with the skin – it is difficult to keep them fully intact and separated from the skin. However, you should be able to identify each.
See images below to help you identify these muscles.
The platysma is a cutaneous muscle that passes from the dorsal median raphe of the neck to the angle of the mouth, where it radiates into the orbicularis oris in the lips. It is the most superficial muscle, covering the ventrolateral surface of the face.
The orbicularis oris lies near the free borders of the lips and extends from one lip to the other around the angle of the mouth. The fibers of each side end at the median plane of both the superior and inferior incisor regions.
The buccinator muscle is a thin, wide muscle that forms the foundation of the cheek. It attaches to the alveolar margins of the mandible and maxilla and the adjacent buccal mucosa. It may be found between the rostral border of the masseter muscle and the orbicularis oris. You can help define the buccinator muscle by placing your finger within the cheek and pressing outward. Dissect deep to the cranial attachment of the platysma to reveal its external surface. A portion of the buccinator lies deep to the orbicularis oris muscle and is difficult to separate from it. It functions to return food from the vestibule to the occlusal surface of the teeth.
The levator nasolabialis is a flat muscle lying beneath the skin on the lateral surface of the maxillary bone. It arises from the maxillary bone, courses rostroventrally, and attaches to the edge of the superior lip and on the naris, the external opening of each half of the nasal cavity. It dilates the nostril and raises the superior lip.
- Superficial muscles of the head of the dog, lateral aspect. 1
The auriculopalpebral nerve arises as the facial nerve curves rostrally ventral to the external acoustic meatus and horizontal ear canal.
Rostral auricular branches course through the parotid gland and are distributed to the rostral auricular muscles. The auriculopalpebral nerve crosses the zygomatic arch, supplies branches to the rostral auricular plexus, and continues to the orbit to supply palpebral branches to the orbicularis oculi m. Beyond this, a branch passes medial to the orbit and continues rostrally on the nose to supply the muscles of the nose and upper lip.
Two buccal branches of the facial nerve course across the masseter muscle to innervate the muscles of the cheek, the superior and inferior lips, and the lateral surface of the nose. The dorsal buccal branch is dorsal to the parotid duct. The ventral buccal branch is ventral to the parotid duct, near the ventral border of the masseter m.
Dissect: Returning to the surface dissection of the masseter muscle, identify the dorsal and ventral buccal branches of the facial nerve running in the fascia covering the muscle (you should see a parotid salivary duct running between them, which results in three structures running in parallel across the lateral surface of the masseter). Follow the branches caudally towards their origin deep to the parotid salivary gland. Retract the parotid salivary gland caudally by carefully dissecting deep to its rostral margin (if not done already), while keeping its duct intact. Then continue tracing the buccal branches deep to the gland and appreciate that they arise from the facial nerve caudal to the horizontal ear canal and external acoustic meatus. Also identify a branch of the facial nerve passing directly dorsally towards the ear and eye – this is the auriculopalpebral n.
- Superficial branches of the facial and trigeminal nerves of the dog, lateral aspect. 1
- Superficial branches of the facial and ttigeminal nerves of the cat. 4
- Superficial nerves of the dog head. 40
Clinical Application:
Cranial Nerve VIII: The Vestibulocochlear Nerve
The vestibulocochlear nerve (CN VIII) enters the internal acoustic meatus and terminates in the membranous labyrinth of the inner ear. It is the nerve involved in balance and hearing. We will discuss this nerve in a later lab when we cover neuroanatomy.
Cranial Nerve IX: The Glossopharyngeal Nerve
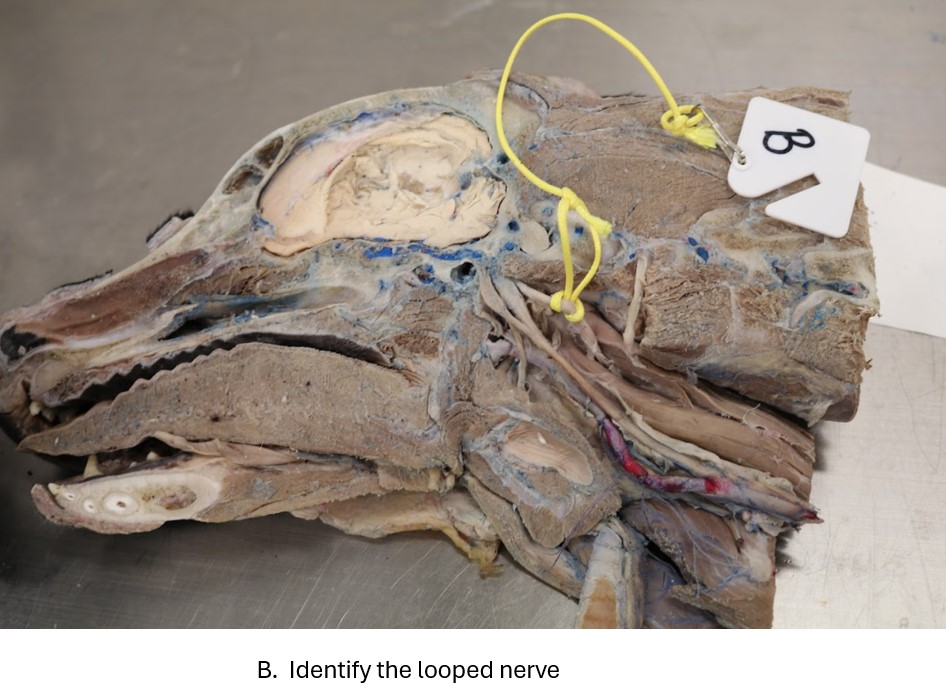
Dissect: We will now move over to the medial side of the head.
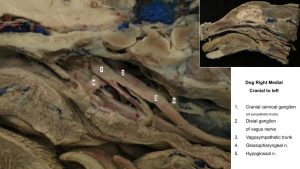
Observation of the ninth, tenth, and eleventh cranial nerves and the sympathetic trunk ganglion at the base of the skull is facilitated by removal of the origin of the digastricus muscle for a lateral view (if not already done). Likewise, removal of the insertion of the longus capitis muscle, and if necessary the rectus capitis ventralis muscle, provides a medial view. Both of these muscle lay on ventral aspect of the atlanto-occipital joint.
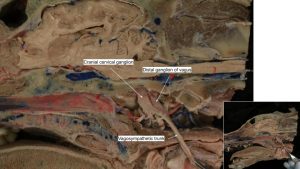
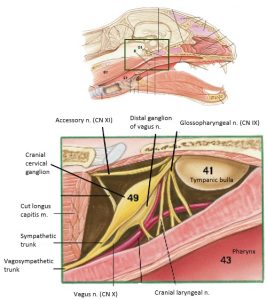
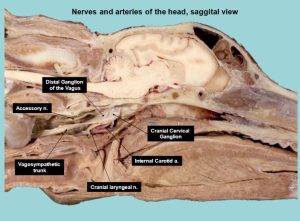
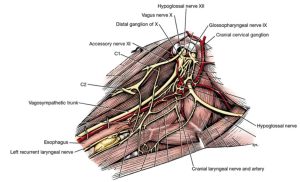
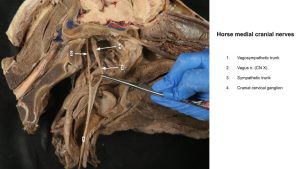
Locate the sympathetic trunk where it is joined with the vagus, forming the vagosympathetic trunk. Follow it cranially to a level ventral and medial to the tympanic bulla, where the two nerves separate. The sympathetic trunk is ventral to the vagus nerve (more on the vagus nerve below).
Trace the sympathetic trunk cranial to the separation and note an enlargement, the cranial cervical ganglion. This is the most cranial group of cell bodies of sympathetic postganglionic axons. These axons are distributed to the smooth muscles and glands of the head via blood vessels and other nerves.
- Removing longus capitis
The glossopharyngeal nerve (CN IX) passes through the jugular foramen and the tympano-occipital fissure. Beyond the fissure the glossopharyngeal n. crosses the lateral surface of the cranial cervical ganglion and divides into pharyngeal and lingual branches that are sensory to the pharyngeal mucosa and motor to the stylopharyngeus and other pharyngeal muscles. In addition, some branches course to the carotid sinus and others contribute to the pharyngeal plexus along with branches of the vagus nerve.
Observe: Observe the glossopharyngeal n. where it crosses the cranial cervical ganglion. You should be able to follow and identify fibers entering the caudodorsal aspect of the muscular pharynx.
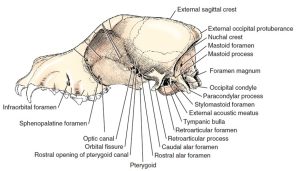
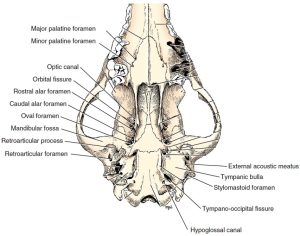
Additionally, identify the tympano-occipital fissure in a skull. You should find this on the ventral side of the skull, just caudal to the tympanic bulla. Note that cranial nerves IX, X, and XI all pass through the tympano-occipital fissure.
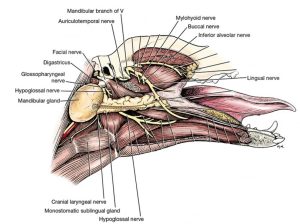
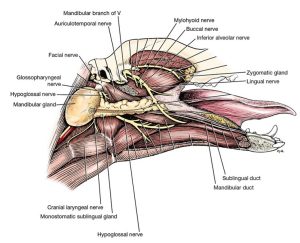
- Nerves and salivary glands medial to right mandible, lateral view, dorsally. 1
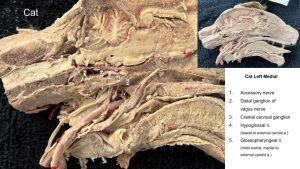
- Cat cranial nerves, medial view. 4
Cranial Nerve X: The Vagus Nerve
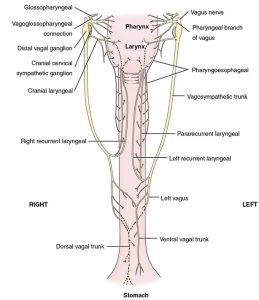
The vagus nerve (CN X) passes through the jugular foramen and the tympano-occipital fissure. It courses along the common carotid artery in the neck with the sympathetic trunk and through the thorax on the esophagus to terminal branches in the thorax and abdomen.
There are two ganglia associated with this nerve. The proximal ganglion of the vagus lies in the jugular foramen and cannot be seen. The distal ganglion of the vagus is found outside the tympano-occipital fissure, ventral and medial to the tympanic bulla and caudal to the cranial cervical ganglion.
Observe: Find the distal ganglion with the vagus nerve caudal to the cranial cervical ganglion on the sympathetic trunk.
The distal ganglion contains the cell bodies of the visceral afferent neurons that are distributed to most of the viscera of the body. Caudal to the distal ganglion, the vagus joins the sympathetic trunk, with which it remains associated throughout its cervical course to the thoracic inlet. The following branches are distributed to cranial cervical structures.
Branches from the vagus and glossopharyngeal nerves and the cranial cervical ganglion form a pharyngeal plexus, which innervates the caudal pharyngeal muscles and the cranial esophagus. The cranial laryngeal nerve leaves the vagus nerve at the distal ganglion and passes ventrally to the larynx, where it supplies the cricothyroid muscle and the laryngeal mucosa.
Observe: Identify the cranial laryngeal nerve as it exits caudally from the distal ganglion of the vagus n.
The origin of the recurrent laryngeal nerve was seen in the thoracic inlet. It innervates the cervical esophagus and trachea in its course up the neck and terminates as the caudal laryngeal nerve, which enters the larynx under the caudal edge of the cricopharyngeus muscle. It innervates all the muscles of the larynx except the cricothyroideus m. We specifically note here that it innervates the cricoarytenoideus dorsalis (CAD) m., but we will not identify the caudal laryngeal nerve.
- Innervation of the esophagus. 1
- Cat cranial nerves, medial view. 4
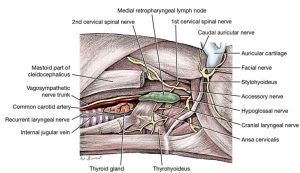
- Retropharyngeal lymph node and thyroid gland, lateral aspect of the neck. 1
- Medial nerves of the dog head. 40
Cranial Nerve XI: The Accessory Nerve
The accessory nerve (CN XI) passes through the jugular foramen and the tympano-occipital fissure along with the ninth and tenth cranial nerves. It passes caudally and by a ventral branch innervates the mastoid part of the sternocephalicus and cleidocephalicus muscles. The dorsal branch supplies the cervical part of the cleidocephalicus and the trapezius.
Observe: Identify the accessory nerve (CN XI) coursing caudally, lateral to the vagus nerve and sympathetic trunk.
- Nerves emerging from tympano-occipital fissure, right lateral view. 1
- Cat cranial nerves, medial view. 4
Cranial Nerve XII: The Hypoglossal Nerve
The hypoglossal nerve (CN XII) passes through the hypoglossal canal. It passes ventrorostrally, lateral to the vagosympathetic trunk and the carotid arteries. It lies medial to the mandibular salivary gland, digastricus, and mandible. The hypoglossal nerve is closely associated with the lingual artery. Deep to the mylohyoideus, it innervates the extrinsic and intrinsic muscles of the tongue. The ansa cervicalis consists of two branches that leave the hypoglossal nerve and join the ventral branch of the first cervical spinal nerve in the region of the hyoid muscles. This provides hypoglossal innervation to the sternothyroid and sternohyoid muscles.
Observe: Identify the hypoglossal nerve as it courses with the lingual artery and follow it dorsally, as it runs lateral to the vagosympathetic trunk and the carotid arteries.
- Nerves emerging from tympano-occipital fissure, right lateral view. 1
- Nerves and salivary glands medial to right mandible, lateral view, dorsally. 1
Deep Dissection
Start here if you are performing the deep dissection.
Dissect: Carefully skin one half of your cadaver’s head. Leave a narrow rim of skin around the margin of the eyelids and at the edge of the lips. Preserve the nose and the philtrum, which is the median groove separating the right and left parts of the nose and superior lips. You need only skin to the base of the ear.
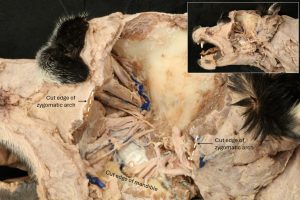
Unlike the half of the team performing the superficial dissection, you need not be as careful to ensure that the superficial muscles, nerves, vessels, and ducts of the face remain intact. In fact, do not waste time preserving the superficial branches of the facial and trigeminal nerves or the parotid duct, as these will be removed along with the masseter muscle. There is a large volume of muscle to be resected in this dissection. Review prosections to observe how deeply the dissection occurs before beginning.
On the lateral aspect of this head half, cut all of the attachments of the temporal and masseter muscles to the zygomatic arch. Cut through the bony arch rostrally and caudally and remove all of the arch rostral to the temporomandibular joint.
Remove the temporalis m. from its wide origin by sharply excising the bulk of it with a scalpel. Once closer to the surface of the skull, muscle can be scraped off the bone with the blunt end of thumb forceps or a scalpel handle (with no blade loaded!). Be vigorous; there is a large amount of muscle to remove.
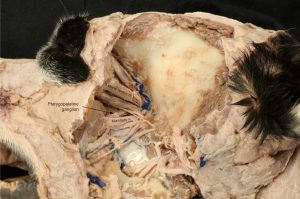
Transect the masseter m. as close to its attachment on the zygomatic arch as possible and use this incision as the starting point to remove the entire masseter m. all the way medially to the coronoid process. With bone cutters, remove most of the zygomatic arch. Now, remove the coronoid process and the remaining attached muscles. As you remove muscle to expose the underlying pterygoid muscles, note that there are a number of important arteries and nerves (the maxillary artery/nerve are the most obvious of these structures) located just lateral (superficial) to the pterygoid muscles that will need to be identified, so proceed with caution. Take a moment to have a look at a prosected deep dissection to guide you through this process. Complete the disarticulation of the temporomandibular joint and reflect the ramus of the mandible laterally, ultimately removing the entire ramus. You may find that there is still some temporalis muscle tissue that needs to be removed in order to readily identify the deeper structures.
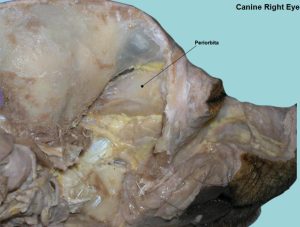
See image below to get a sense of the view that you should be able to see in your cadaver. Arteries and nerves passing over the shiny white fascia of the pterygoid muscles indicates that you are deep enough! In the cat, you will notice what looks to be a red splotch of small arteries. This is the rete mirabile maxillaris, and replaces the maxillary artery in this location in the cat! Behind the eye orbit you should find a dull, white, fibrous tissue. This is the periorbita and we’ll leave it intact for now.
Cranial Nerve I: The Olfactory Nerve
The olfactory nerve (CN I) consists of numerous axons that arise in the olfactory epithelium of the caudal nasal mucosa and pass through the cribriform foramina to the olfactory bulbs. These include axons from the vomeronasal organ that course along the nasal septum. No dissection is necessary.
Looking at the medial surface of the bisected head, note the olfactory bulb sitting the most rostral part of the neurocranium, just dorsal to the cribiform plate.
- Sagittal section of the nose to show distribution of nerves 3
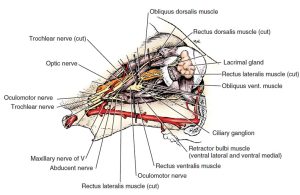
Cranial Nerve II: The Optic Nerve
The optic nerve (CN II) is also referred to as the “prechiasmatic optic tract”. It is surrounded by the retractor bulbi muscle within the periorbita as it enters the caudal aspect of the bulbus oculi (eyeball). It is responsible for the special sense of vision.
The periorbita is a cone-shaped sheath of connective tissue and smooth muscle that encloses the eyeball and its muscles, vessels, and nerves. Where the periorbita contacts the bone medially, it is the periosteum of the orbit. Its apex is caudal where it attaches to the bony margin of the optic canal and the orbital fissure. Here it is continuous with the dura intracranially. Rostrally, it widens to blend with the periosteum of the face. Orbital fat may be observed on both sides of the periorbita.
Dissect: Removal of the temporal muscle on your deep dissection should have exposed the periorbita. If it didn’t, remove more temporal muscles until the periorbita is exposed. Reflect the orbital ligament and the periorbita from the dorsolateral surface of the eyeball. Incise the periorbita longitudinally on its lateral side and reflect it to expose the eyeball muscles and the levator of the superior eyelid.
Observe: Observe the large optic nerve (i.e., the optic tract) in the periorbita and as it enters the optic canal. It will be found deep to the extraocular muscles and can be hooked with a blunt probe to better visualize it.
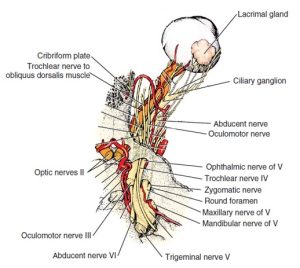
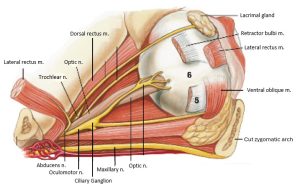
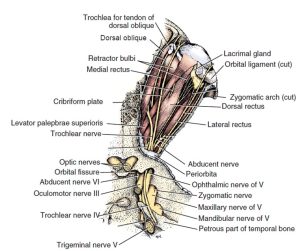
- Schema of the optic, oculomotor, trochlear, trigeminal (ophthalmic nerve) and abducent nerves, dorsal aspect. 3
- Nerves of the eye and orbit, lateral aspect. 3
- Cranial nerves of the orbital region of the cat. 4
- Dog periorbita. 40
Cranial Nerve III: The Oculomotor Nerve
The oculomotor nerve (CN III) passes through the orbital fissure and enters the periorbita with the optic n. The oculomotor nerve innervates the dorsal, medial, and ventral recti mm.; the ventral oblique m.; and the levator palpebrae superioris m. The ciliary ganglion is an irregular enlargement at the termination of the oculomotor nerve on the ventral surface of the middle of the optic nerve. This ganglion contains parasympathetic cell bodies of postganglionic axons that innervate the sphincter pupillae of the iris. It functions to regulate the size of the pupil in response to the amount of light entering the eye and in accommodation.
Observe: Identify the lateral rectus, dorsal rectus, ventral rectus, and retractor bulbi muscles deep to the periorbita. Locate the ciliary ganglion just ventral to the optic nerve (see images below to orient yourself). Reflection of the lateral rectus m. and retractor bulbi m. may be necessary.
- Schema of the optic, oculomotor, trochlear, trigeminal (ophthalmic nerve) and abducent nerves, dorsal aspect. 3
- Nerves of the eye and orbit, lateral aspect. 3
- Cranial nerves of the orbital region of the cat. 4
Cranial Nerve IV: The Trochlear Nerve
The trochlear nerve (CN IV) also passes through the orbital fissure and enter the periorbita. It innervates the dorsal oblique m. and need not be dissected.
- Superficial distribution of the nerves of the eye, dorsal aspect. 3
- Schema of the optic, oculomotor, trochlear, trigeminal (ophthalmic nerve) and abducent nerves, dorsal aspect. 3
- Nerves of the eye and orbit, lateral aspect. 3
Cranial Nerve V: The Trigeminal Nerve
The trigeminal nerve (CN V) divides into three nerves as it emerges from the trigeminal canal in the petrosal part of the temporal bone: the ophthalmic (V1), the maxillary (V2), and the mandibular (V3) nerves. We’ll discuss each of these in turn.
Ophthalmic n. (V1)
The ophthalmic n. passes through the orbital fissure and supplies sensory nerves that enter the periorbita. The ophthalmic n. and its branches need not be dissected. The frontal and infratrochlear nerves pass rostrally between the dorsal oblique and dorsal rectus muscles to innervate the medial aspect of the superior and inferior eyelids. Long ciliary nerves follow the optic nerve and innervate the eyeball. The ethmoidal nerve passes through an ethmoidal foramen and the cribriform plate to innervate the nasal mucosa and skin of the nose.
- Superficial distribution of the nerves of the eye, dorsal aspect. 3
- Schema of the optic, oculomotor, trochlear, trigeminal (ophthalmic nerve) and abducent nerves, dorsal aspect. 3
Maxillary n. (V2)
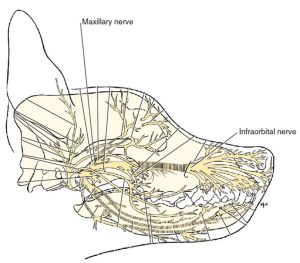
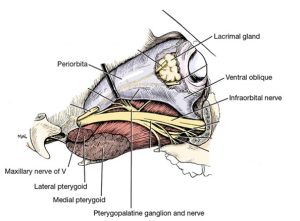
The maxillary nerve (V2) enters the alar canal through the round foramen. It emerges from the rostral alar foramen and crosses the pterygopalatine fossa dorsal to the pterygoid muscles and ventral to the periorbita, accompanied by the maxillary artery.
The infraorbital nerve is the continuation of the maxillary nerve in the pterygopalatine fossa (a small nerve called the caudal nasal n. separates from the maxillary n. midway across the medial pterygoid m., at which point the maxillary n. becomes known as the infraorbital n.). The infraorbital n. enters the infraorbital canal through the maxillary foramen. Along its course through the infraorbital canal, it gives off superior alveolar branches, which supply the roots of the teeth of the superior arcade via the alveolar canals. As the infraorbital nerve emerges from the infraorbital foramen, it divides into a number of fasciculi, which are distributed to the skin and adjacent structures of the superior lip and nose.
Dissect: Dissect the maxillary n. coursing across the medial pterygoid m. and the infraorbital n. entering the maxillary foramen. The maxillary n. passes with the large maxillary artery in a dog. In a cat, you should be able to trace the maxillary nerve rostrally from the rete mirabile maxillaris towards the maxillary foramen.
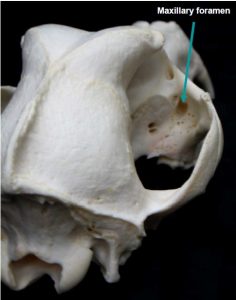
Observe: On a skull, identify the maxillary foramen, infraorbital canal, and infraorbital foramen by passing a pipe cleaner through the entire canal. This pipe cleaner reflects the path of the infraorbital n.
- Path of the maxillary nerve in the dog. 1
- Schematic illustration of the primary branches of the trigeminal nerve in the cat. 7
- Dog skull with calvaria removed, dorsal aspect. 1
- Maxillary branch of trigeminal nerve, lateral aspect. 1
- Cranial nerves of the orbital region of the cat. 4
- Superficial branches of the facial and trigeminal nerves of the dog, lateral aspect. 1
- Muscles of the eyeball of the dog. 1
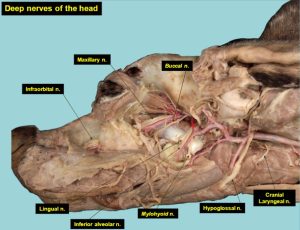
- Deep nerves of the dog head. 440
Clinical Application
Dental nerve blocks, pt. 1: The Upper Teeth
It is frequently necessary to perform dental procedures on our patients; be it cleanings, extractions, tooth filings, etc. To aid in pain management during these procedures, application of an anesthetic to the particular that innervates the affected tooth row(s) is a necessary step for most veterinarians.
For the upper teeth, the primary nerve responsible for their sensory innervation is the maxillary nerve and one of its primary branches, the infraorbital nerve. Blocking the maxillary nerve will desensitize the entirety of the ipsilateral upper arcade (i.e., all of the upper teeth on the same side as the nerve). The approach for blocking this nerve involves placing a needle behind the last maxillary molar to drop the anesthetic on the maxillary nerve right before it enters the maxillary foramen.
- Maxillary nerve block
- Maxillary nerve block
- Maxillary nerve block
Blocking the infraorbital nerve (often called a “rostral maxillary nerve block“) blocks the upper incisors, canine, and first two premolars on the ipsilateral side. However, in most cats and in brachycephalic breeds in general, a rostral maxillary nerve block can desensitize all of the upper teeth on the ipsilateral side. This is because of the short length of the infraorbital canal, with the anesthetic effectively diffusing across the entire canal. The approach for blocking this nerve involves placement of the needle into the infraorbital foramen.
- Infraorbital nerve block
- Infraorbital nerve block
- Infraorbital nerve block
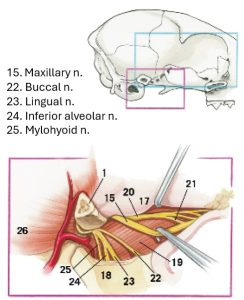
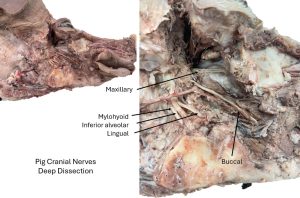
Mandibular n. (V3)
The mandibular nerve exits the neurocranium via the oval foramen. The deep branches of the mandibular nerve should have been exposed by the deep dissection through the temporal muscle to expose the pterygoid muscles and periorbita completed previously. Please note an important branch of the mandibular nerve is also seen in the superficial dissection.
Branches arise on the surface of the pterygoid muscles’ ventral and lateral to the apex of the periorbita. These include the pterygoid, deep temporal, and masseteric nerves that contain somatic motor neurons that innervate these muscles of mastication. Most of these branches have been severed by the dissection. The buccal nerve crosses the pterygoid muscles just ventral to the maxillary n. and enters the cheek lateral to the zygomatic salivary gland. This nerve is sensory to the mucosa and skin of the cheek.
Observe: Locate the buccal nerve just ventral to the maxillary n., crossing over the lateral surface of the pterygoid muscles.
Coursing rostroventrally from the oval foramen, the mandibular n. has three branches that pass medial to the body of the mandible. These are the lingual, inferior alveolar, and mylohyoid nerves.
The lingual nerve (sensory) is the largest and most rostral of the three. It can be observed coursing across the pterygoid muscles and passing between the styloglossus and mylohyoideus. It is sensory to the rostral two thirds of the tongue.
The inferior alveolar nerve enters the mandibular foramen on the medial side of the ramus of the mandible. It courses through the mandibular canal, supplying sensory nerves to the teeth. The mental nerves that emerge through the mental foramina and supply the lower lip are branches from this nerve.
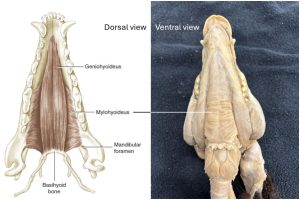
The mylohyoid nerve is a caudal branch of the inferior alveolar n. It reaches the ventral border of the mandible, supplies a branch to the rostral belly of the digastricus muscle, and continues into the mylohyoideus muscle. It is motor to the mylohyoideus m. and sensory to the skin between the mandibles.
Dissect: Where you removed the ramus of the mandible, observe the lingual, inferior alveolar, and mylohyoid nerves, which cross the dorsolateral surface of the medial pterygoid muscle.
Observe: Identify the mandibular foramen and mental foramina on a mandible. The mandibular foramen is seen on the medial aspect of the mandibular ramus; the mental foramina are seen on the rostral, lateral aspect of the body of the mandible. The mandibular canal connects these foramina.
- Nerves and salivary glands of the dog medial to right mandible, lateral view. 1
- Schematic illustration of the primary branches of the trigeminal nerve in the cat. 7
- Deep branchs of the trigeminal nerve of the cat. Lateral view. 4
- Left and right mandibles of the dog, dorsal lateral aspect. 1
- Muscles of the dog mandible and basihyoid bone. 1
- Deep nerves of the dog head. 440
- Deep nerves of the dog head. 40
Clinical Application
Dental Nerve Blocks, pt. 2: The Lower Teeth
For the lower teeth, the primary nerve responsible for their innervation is the inferior alveolar nerve, a branch of the mandibular nerve. The inferior alveolar nerve provides innervation to all of the mandibular teeth on the ipsilateral side. Blocking the inferior alveolar nerve involves injection of anesthetic to the nerve before it passes into the mandibular foramen. There are two approaches to this nerve block; an extraoral and intraoral technique.
- Inferior alveolar nerve block
- Inferior alveolar nerve block
- Inferior alveolar nerve block
The mental nerves are branches of the inferior alveolar nerve that exit the mandibular canal via the mental foramina. Blocking the middle mental nerve desensitizes the mandibular incisors and canine on the ipsilateral side. Placement of the needle should be in the mental foramen.
- Mental nerve block
- Mental nerve block
- Mental nerve block
Cranial Nerve VI: The Abducent Nerve
The abducent nerve (CN VI) passes through the orbital fissure and enters the periorbita. It innervates the retractor bulbi and the lateral rectus mm.
Dissect: Identify the lateral rectus and retractor bulbi muscles. Bluntly dissect the abducent nerve as it enters the belly of the lateral rectus m.
- Superficial distribution of the nerves of the eye, dorsal aspect. 3
- Nerves of the eye and orbit, lateral aspect. 3
- Cranial nerves of the orbital region of the cat. 4
Cranial Nerve VII: The Facial Nerve
The facial nerve (CN VII) innervates all of the superficial muscles of facial expression, the caudal belly of the digastricus muscle, and the platysma m. of the neck. The nerve enters the petrosal part of the temporal bone through the internal acoustic meatus, courses through the facial canal of that bone, and leaves the skull at the stylomastoid foramen just caudal to the external acoustic meatus, where it divides into several branches.
The pterygopalatine ganglion is a ganglion associated with the facial n. (CN VII) and is found just dorsal to the maxillary nerve on the surface of the medial pterygoid muscle. It contains cell bodies of postganglionic parasympathetic axons that supply the lacrimal, nasal, and palatine glands. The postganglionic axons course with the branches of the maxillary nerve to their terminations.
Dissect: Reflect the periorbita dorsally and the maxillary nerve ventrally to see this small, flat ganglion on the medial pterygoid muscle.
- Maxillary branch of trigeminal nerve, lateral aspect. 1
Cranial Nerve VIII: The Vestibulocochlear Nerve
The vestibulocochlear nerve (CN VIII) enters the internal acoustic meatus and terminates in the membranous labyrinth of the inner ear. It is the nerve involved in balance and hearing. We will see this nerve in a later lab when we cover neuroanatomy.
Cranial Nerve IX: The Glossopharyngeal Nerve
Dissect: We will now move over to the medial side of the head.
Observation of the ninth, tenth, and eleventh cranial nerves and the sympathetic trunk ganglion at the base of the skull is facilitated by removal of the origin of the digastricus muscle for a lateral view (if not already done). Likewise, removal of the insertion of the longus capitis muscle, and if necessary the rectus capitis ventralis muscle, provides a medial view.
Locate the sympathetic trunk where it is joined with the vagus, forming the vagosympathetic trunk. Follow it cranially to a level ventral and medial to the tympanic bulla, where the two nerves separate. The sympathetic trunk is ventral to the vagus nerve (more on the vagus nerve below).
Trace the sympathetic trunk cranial to the separation and note an enlargement, the cranial cervical ganglion. This is the most cranial group of cell bodies of sympathetic postganglionic axons. These axons are distributed to the smooth muscles and glands of the head via blood vessels and other nerves.
- Removing longus capitis
The glossopharyngeal nerve (CN IX) passes through the jugular foramen and the tympano-occipital fissure. Beyond the fissure the glossopharyngeal n. crosses the lateral surface of the cranial cervical ganglion and divides into pharyngeal and lingual branches that are sensory to the pharyngeal mucosa and motor to the stylopharyngeus and other pharyngeal muscles. In addition, some branches course to the carotid sinus and others contribute to the pharyngeal plexus along with branches of the vagus nerve.
Observe: Observe the glossopharyngeal n. where it crosses the cranial cervical ganglion. You should be able to find branches entering the caudo-dorsal aspect of the pharyngeal muscles.
- Nerves and salivary glands medial to right mandible, lateral view, dorsally. 1
- Cat cranial nerves, medial view. 4
Cranial Nerve X: The Vagus Nerve
The vagus nerve (CN X) passes through the jugular foramen and the tympano-occipital fissure. It courses along the common carotid artery in the neck with the sympathetic trunk and through the thorax on the esophagus to terminal branches in the thorax and abdomen.
There are two ganglia associated with this nerve. The proximal ganglion of the vagus lies in the jugular foramen and cannot be seen. The distal ganglion of the vagus is found outside the tympano-occipital fissure, ventral and medial to the tympanic bulla and caudal to the cranial cervical ganglion.
Observe: Find the distal ganglion with the vagus nerve caudal to the cranial cervical ganglion on the sympathetic trunk.
The distal ganglion contains the cell bodies of the visceral afferent neurons that are distributed to most of the viscera of the body. Caudal to the distal ganglion, the vagus joins the sympathetic trunk, with which it remains associated throughout its cervical course to the thoracic inlet. The following branches are distributed to cranial cervical structures.
Branches from the vagus and glossopharyngeal nerves and the cranial cervical ganglion form a pharyngeal plexus, which innervates the caudal pharyngeal muscles and the cranial esophagus. The cranial laryngeal nerve leaves the vagus nerve at the distal ganglion and passes ventrally to the larynx, where it supplies the cricothyroid muscle and the laryngeal mucosa.
Observe: Identify the cranial laryngeal nerve as it exits caudally from the distal ganglion of the vagus n.
The origin of the recurrent laryngeal nerve was seen in the thoracic inlet. It innervates the cervical esophagus and trachea in its course up the neck and terminates as the caudal laryngeal nerve, which enters the larynx under the caudal edge of the cricopharyngeus muscle. It innervates all the muscles of the larynx except the cricothyroideus m. We specifically note here that it innervates the cricoarytenoideus dorsalis (CAD) m.
- Innervation of the esophagus. 1
- Cat cranial nerves, medial view. 4
- Retropharyngeal lymph node and thyroid gland, lateral aspect of the neck. 1
- Medial nerves of the dog head. 40
Cranial Nerve XI: The Accessory Nerve
The accessory nerve (CN XI) passes through the jugular foramen and the tympano-occipital fissure along with the ninth and tenth cranial nerves. It passes caudally and by a ventral branch innervates the mastoid part of the sternocephalicus and cleidocephalicus muscles. The dorsal branch supplies the cervical part of the cleidocephalicus and the trapezius.
Observe: Identify the accessory nerve (CN XI) coursing caudally, lateral to the vagus nerve and sympathetic trunk.
- Nerves emerging from tympano-occipital fissure, right lateral view. 1
- Cat cranial nerves, medial view. 4
Cranial Nerve XII: The Hypoglossal Nerve
The hypoglossal nerve (CN XII) passes through the hypoglossal canal. It passes ventrorostrally, lateral to the vagosympathetic trunk and the carotid arteries. It lies medial to the mandibular salivary gland, digastricus, and mandible. The hypoglossal nerve is closely associated with the lingual artery. Deep to the mylohyoideus, it innervates the extrinsic and intrinsic muscles of the tongue. The ansa cervicalis consists of two branches that leave the hypoglossal nerve and join the ventral branch of the first cervical spinal nerve in the region of the hyoid muscles. This provides hypoglossal innervation to the sternothyroid and sternohyoid muscles.
Observe: Identify the hypoglossal nerve as it courses with the lingual artery and follow it dorsally, as it runs lateral to the vagosympathetic trunk and the carotid arteries.
- Nerves emerging from tympano-occipital fissure, right lateral view. 1
- Nerves and salivary glands medial to right mandible, lateral view, dorsally. 1
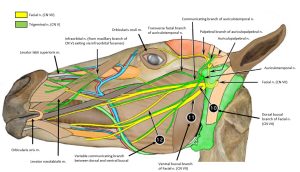
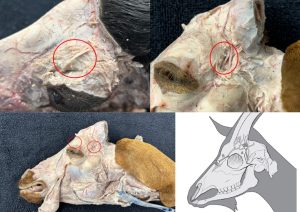
The Ungulate Perspective
Observe: Identify the following structures (see bullet point list below) in the instructors’ ungulate prosections. As a general rule, the cranial nerves and their branches tend to follow the same pathways that we see in the carnivore…exceptions to this are noted below.
- Optic n. (CN II)
- Dorsal rectus (innervated by CN III), ventral rectus (CN III), lateral rectus mm (CN VI)
- Trigeminal n. (CN V)
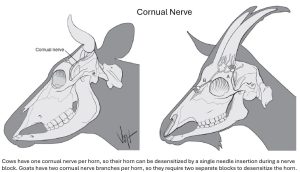
- Cornual nn.; (these nerves innervate the base of the horn of the goat and ox) – branch of Ophthalmic n.
- Maxillary n. (seen on a deep dissection)
- Infraorbital n.
- Mandibular n.
- Auriculotemporal n.; *Note that the auriculotemporal n. in the ungulate tends to “hitch a ride” with the dorsal buccal br. of CN VII*
- Inferior alveolar n.
- Mental n.
- Superficial branchs of facial and trigeminal nerves of the horse, lateral view. 2
- Branches of facial and trigeminal nerves of the ox, lateral view. 2
- Schematic illustration of the primary branches of the mandibular nerve in the horse without the deep temporal nerves. 7
- Horse facial mm
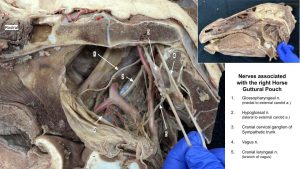
- Dissection of a horse head showing deep branches of the Trigeminal nerve (CN V), specifically the Maxillary and Mandibular nerves.
- Horse deep cranial nerves
- horse eye
- Cornual nerve differences in ruminants. Food Animal Surgery
- Goat cornual nerve
- Superficial goat nerves. 40
- Superficial goat nerves. 40
- Deep dissection of the pig, showing the trigeminal nerve branches
Clinical application
Dehorning is a routine aspect of ruminant medicine – performed on nearly every dairy cow and dairy goat. To desensitize the horn or horn bud, the cornual nerve is blocked. Cows have one branch of the cornual nerve, which can frequently be palpated as it crosses over the temporal line. Goats have two branches of the cornual nerve. In mature animals, additional desensitization can be achieved with a ring block around the horn.
- Facial n. (CN VII)
- Dorsal/ventral buccal branches of CN VII; *Note that the ventral buccal branch in the goat, calf, and pig courses along the ventral border of the masseter m.*
- Facial muscles to identify: Oribicularis oculi; orbicularis oris, levator nasolabialis, levator labii superioris
- Levator labii superioris is the “laugh muscle” in the horse, and covers the infraorbital foramen. Therefore it is displaced dorsally to palpate the foramen for nerve blocks. In the pig, the muscle attaches to the os rostri.
- Identify the platysma m. in the pig
- Auriculopalpebral n.
- Muscles of facial expression of the ox. 2
- Selected structures of the pig head, lateral view. 2
- Superficial facial muscles of the horse. 11
- Superficial nerves and muscles of the ox. 11
- Superficial nerves and muscles of the goat. 11
- Superficial nerves and muscles of the pig. 11
- Horse facial mm
- Glossopharyngeal n. (CN IX)
- Branches dive into the dorsal aspect of pharynx, just like in carnivore
- Vagus n. (CN X)
- Cranial laryngeal n.
- Innervates cricothyroideus m. (don’t identify muscle)
- Caudal laryngeal n.
- Just like the carnivore, we will not identify this nerve, but know that it innervates the cricoarytenoideus dorsalis (CAD) m.
- Cranial laryngeal n.
- Sympathetic trunk
- Cranial cervical ganglion
- Vagosympathetic trunk
- Accessory n. (CN XI)
- Hypoglossal n. (CN XII)
- Innervates muscles of the tongue
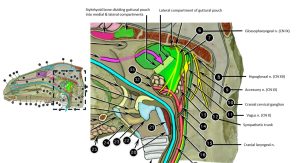
- Horse guttural pouch region, medial view. 2
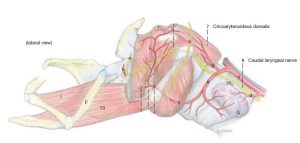
- Innervation to the horse larynx, lateral view. 14
Review Videos
Carnivore cranial nerves (Spradley) – 19 min
Carnivore cranial nerves (Gerard) – 28 min
Ungulate cranial nerves – 16 min
Terms
| Terms | Species |
| Olfactory n. (CN I) | ID the olfactory bulb, but we won’t identify a single “olfactory n.” |
| Olfactory bulb | All |
| Cribiform plate | Canine skull |
| Optic n. (CN II) | All |
| Optic canal | Canine skull |
| Periorbita | All; fibrous tissue that surrounds the extraocular mm. |
| Oculomotor n. (CN III) | Carnivore |
| Orbital fissure | Canine skull; transmits CNs III, IV, ophthalmic br. of V, and VI |
| Ciliary ganglion | Carnivore |
| Dorsal rectus m. | All |
| Ventral rectus m. | All |
| Medial rectus m. | Know that it is innervated by CN III, but we will not identify it. |
| Ventral oblique m. | Know that it is innervated by CN III, but we will not identify it. |
| Trochlear n. (CN IV) | Know the muscle it innervates (dorsal oblique m.) |
| Trigeminal n. (CN V) | We will ID branches, not the trigeminal n. as a single nerve. |
| Ophthalmic n. (V1) | Know what region of the face it innervates, but do not identify |
| Maxillary n. (V2) | All |
| Round foramen | Canine skull |
| Alar canal | Canine skull |
| Infraorbital n. | All |
| Maxillary foramen | Identify on skull |
| Infraorbital canal | Identify on skull |
| Infraorbital foramen | Identify on skull |
| Cornual nn. | Goat |
| Mandibular n. (V3) | All |
| Auriculotemporal n. | All |
| Buccal n. | Carnivore |
| Lingual n. | Carnivore |
| Inferior alveolar n. | Carnivore |
| Mylohyoid n. | Carnivore |
| Mandibular foramen | Identify on skull |
| Mandibular canal | Identify on skull |
| Mental foramina | Identify on skull |
| Abducent n. (CN VI) | Carnivore |
| Lateral rectus m. | All |
| Retractor bulbi m. | Carnivore |
| Facial n. (CN VII) | Understand, but we don’t see the facial n. by itself (just its branches, see below) |
| Dorsal buccal br. | All |
| Ventral buccal br. | All |
| Auriculopalpebral n. | All |
| Pterygopalatine ganglion | All |
| Platysma m. | Carnivore; pig |
| Orbicularis oris m. | All |
| Buccinator m. | Carnivore |
| Orbicularis oculi m. | All |
| Levator nasolabialis m. | All |
| Levator labii superioris m. | Ungulates |
| Vestibulocochlear n. (CN VIII) | Understand, don’t identify |
| Glossopharyngeal n. (CN IX) | All |
| Tympano-occipital fissure | Canine skull; transmits CNs IX, X, and XI |
| Vagus n. (CN X) | All |
| Distal ganglion of vagus | All |
| Cranial laryngeal n. | All; innnervates cricothyroideus m. |
| Caudal laryngeal n. | Know what muscle it innervates (CAD m.), but do not identify |
| Vagosympathetic trunk | All |
| Accessory n. (CN XI) | All |
| Hypoglossal n. (CN XII) | All; innervates tongue, follows lingual artery rostrally |
| Sympathetic trunk | Understand as component of vagosympathetic trunk |
| Cranial cervical ganglion | All; last opportunity for sympathetic fibers to synapse with post-ganglionic partner cranially |