Lab 15A: Special Senses
Learning Objectives
- Identify the parts of the external ear.
- Identify the superficial structures of the eye (i.e., eye adnexa).
- Identify the periorbita and extraocular mm. Name the action and innervation of each extraocular mm.
- Name and identify the 3 tunics of the eyeball (bulbus oculi), and the structures associated with each tunic.
- Name and identify the chambers of the eye, and the fluids associated with each chamber.
- Identify the lens and its associated structures.
Lab Instructions:
The External Ear
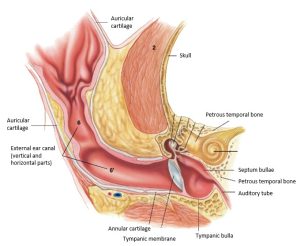
The external ear consists of the auricle and the external acoustic meatus (i.e., the ear canal). The external acoustic meatus is mostly cartilaginous but has a short osseous part on the lateral aspect of the tympanic bulla. The cartilaginous part of the meatus makes a right-angle turn in the deeper part of its course and extends to the tympanic membrane.
Except for one small annular cartilage adjacent to the skull, the external ear consists of a single auricular cartilage that is rolled into a tube ventromedially. The tubular part becomes the external acoustic meatus.
The auricular cartilage is funnel-shaped. Its external, convex surface faces caudally; its internal, concave surface faces rostrally. It has a slightly folded medial and lateral margin called the helix. The auricular cartilage is thin and pliable except proximally, where it thickens and rolls into a tube. On its internal, concave wall at the level of the beginning of the external acoustic meatus, there is a transverse ridge, the anthelix. Opposite the anthelix the rostral boundary of the initial part of the ear canal is formed by a thick, quadrangular plate of the auricular cartilage, the tragus. Projecting caudally from the tragus and completing the lateral boundary of the external ear canal is a thin, elongate piece of cartilage, the antitragus.
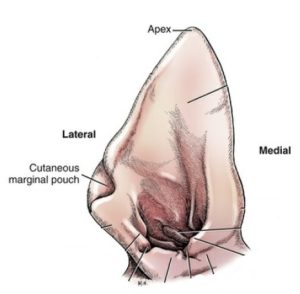
The lateral portion of the helix is indented proximally by an incisure. At this point the skin forms a pouch, the marginal cutaneous sac.
The medial helix is nearly straight. An abrupt angle in this border at its proximal end forms the spine of the helix. Between the spine of the helix and the tragus the medial border of the ear canal is formed by two curved portions of the cartilage, the medial and lateral crura of the helix. They both end laterally in a free border separated from the tragus by the pretragic incisure.
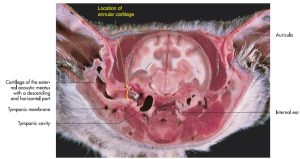
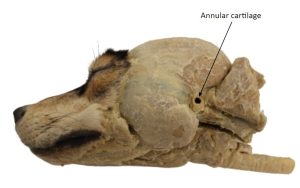
Interposed between the auricular cartilage and the bony external acoustic meatus of the temporal bone is the annular cartilage. This is a band of cartilage that overlaps the bony projection of the meatus. The annular cartilage can be observed on some of the skulls in lab. It is not necessary to dissect it on cadavers, but do identify it on prosected lab specimens.
Observe: Identify the structures of the external ear on the terms chart above on your cadavers and with plastinated models in the lab.
- External canine ear (pinna) showing the Apex, Lateral and Medial surfaces, and the Cutaneous marginal pouch.
- Transverse section through the external ear canal of the cat. 4
- Transverse section of the head of a cat at the level of the ear. 7
- Annular cartilage
- Ticks in the marginal cutaneous sac. B. Black
The Eye Adnexa
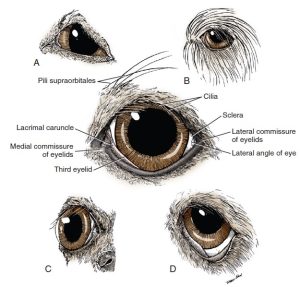
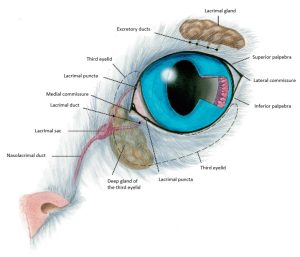
The superior and inferior palpebrae (i.e, the upper and lower eyelids) border the palpebral fissure (the space between the eyelids). They join at either end of the fissure to form the medial and lateral palpebral commissures. Each commissure is attached by ligaments to adjacent bone. The medial palpebral ligament is well developed and attaches the medial commissure to the frontal bone near the nasomaxillary suture. The lateral palpebral ligament is poorly developed and attaches to the zygomatic bone at the orbital ligament.
The upper eyelid bears cilia (eyelashes) on its free border. The lower eyelid lacks cilia. The cutaneous or external surface of the eyelid is covered by hair. The posterior or inner surface is covered by a mucous membrane, the palpebral conjunctiva.
Observe: Follow the palpebral conjunctiva posteriorly to its reflection from the eyelids onto the globe of the eye, which is the bulbar conjunctiva.
The angle formed by this reflection is called the fornix. The cavity thus formed, the conjunctival sac, is open rostrally at the palpebral fissure. It is bounded externally by the palpebral conjunctiva and internally by the bulbar conjunctiva adjacent to the sclera.
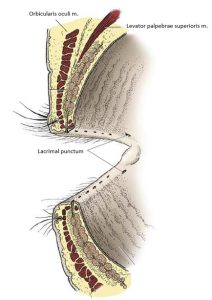
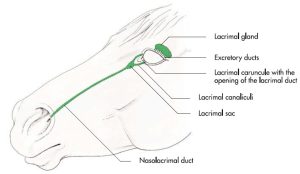
The lacrimal punctum of each lid is the beginning of the dorsal and ventral lacrimal ducts. Each is a small opening on the conjunctival margin of the lid a few millimeters from the medial commissure. The puncta may be difficult to see without the aid of magnification. They are easier to see in a live dog. The lacrimal gland, located ventral to the zygomatic process of the frontal bone secretes through many duct openings into the dorsolateral part of the conjunctival sac. After this serous fluid has passed across the cornea, it is collected by the puncta and passes in succession through the lacrimal duct of each lid, the lacrimal sac, and the nasolacrimal duct to the ventral nasal meatus of the rostral part of each nasal cavity. There, evaporation of the lacrimal secretion takes place. A significant contribution to tear secretion comes from the superficial gland of the third eyelid, conjunctival goblet cells, and tarsal glands of the eyelids. The lacrimal gland and the rostral opening of the nasolacrimal duct will be seen later.
Observe: Review the tear pathway:
Tear glands → dorsal/ventral → lacrimal puncta → dorsal/ventral lacrimal ducts → lacrimal sac → nasolacrimal duct → rostral opening of the nasolacrimal duct (rostral nasal cavity)
- The eyelids of the dog. A, Bull Terrier. B, English Sheepdog. C, Boston Terrier. D, St. Bernard. 1
- Eyelids, sectioned and viewed obliquely from behind. 8
- Sagittal section of the eyeball of the dog. 1
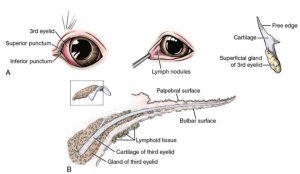
- A, Third eyelid of left eye of the dog. B, Section of the third eyelid. 1
- Tear pathway of the cat. 4
- Lacrimal apparatus of the horse. 7
The plica semilunaris, or third eyelid, is a concave fold of palpebral conjunctiva and cartilage that protrudes from the medial angle of the eye. The cartilage is T-shaped, with an expanded portion in the medial canthus and a stem that extends ventrally into the orbit. It is surrounded by a body of fat and glandular tissue, the superficial gland of the third eyelid. This will be dissected shortly. Its serous secretion enters the conjunctival sac under the third eyelid at the medial commissure.
Observe: Lift the third eyelid from the bulbar conjunctiva and examine its bulbar (lateral) surface.
There are several muscles associated with the eyelids. The orbicularis oculi m. lies partly in the eyelids and is attached medially to the medial palpebral ligament. Laterally, the fibers of the muscle blend with those of the retractor anguli oculi lateralis, which covers the lateral palpebral ligament. The action of the muscle is to close the palpebral fissure. The levator palpebrae superioris m. arises deep within the orbit and will be dissected with the muscles of the eyeball. It elevates the superior lid.
The orbit is a conical cavity containing the eyeball and ocular adnexa. These were exposed when the muscles of mastication were dissected. The orbital margin is formed by the frontal, lacrimal, maxillary, and zygomatic bones and the orbital ligament laterally. The medial wall of the orbit is formed by parts of the frontal, presphenoid, and lacrimal bones. The ventral wall includes the zygomatic salivary gland and the pterygoid muscles. The dorsal and lateral walls are formed primarily by temporal muscle.
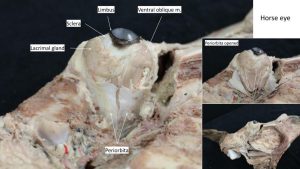
The periorbita is a cone-shaped sheath of connective tissue and smooth muscle that encloses the eyeball and its muscles, vessels, and nerves. Where the periorbita contacts the bone medially, it is the periosteum of the orbit. Its apex is caudal where it attaches to the bony margin of the optic canal and the orbital fissure. Here it is continuous with the dura intracranially. Rostrally, it widens to blend with the periosteum of the face. Orbital fat may be observed on both sides of the periorbita.
Dissect: Removal of the temporalis muscle on your deep dissection should have exposed the periorbita. If it didn’t, remove more temporal muscles until the periorbita is exposed. Reflect the orbital ligament and the periorbita from the dorsolateral surface of the eyeball.
The lacrimal gland is a small, flat lobular structure lying on the medial side of the orbital ligament within the periorbita. Small ducts that cannot be seen without a microscope empty their secretions into the conjunctival sac at the dorsal fornix.
Dissect: Incise the periorbita longitudinally on its lateral side and reflect it to expose the eyeball muscles and the levator of the superior eyelid.
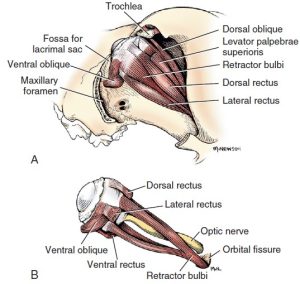
The levator palpebrae superioris m. is thin, narrow, and superficial. It begins at the apex of the orbit, extends over the dorsal rectus m., and widens to insert as a flat tendon in the superior eyelid. It is innervated by the oculomotor nerve (cranial nerve III).
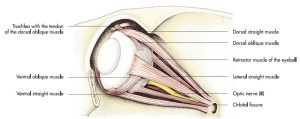
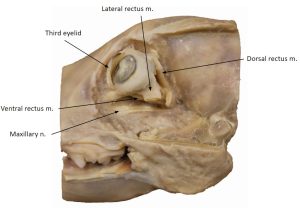
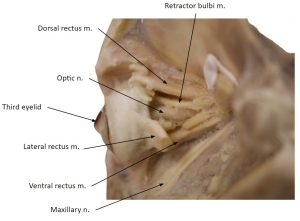
There are seven extrinsic muscles of the eyeball: two obliquus muscles, four rectus muscles, and the retractor bulbi. All of these extrinsic muscles insert on the fibrous coat of the eyeball, the sclera, near the equator of the eyeball. The rectus muscles insert closer to the corneoscleral junction than the retractor muscles.
The four rectus muscles are the dorsal rectus, medial rectus, ventral rectus, and lateral rectus mm.. As they course rostrally from their small area of origin around the optic canal and orbital fissure, they diverge and attach to the sclera on an imaginary line encircling the eyeball at its equator. In the spaces between the rectus muscles, parts of the retractor bulbi can be seen. The retractor bulbi muscle consists of four fascicles that surround the prechiasmatic optic tract (optic nerve), a dorsal pair and a ventral pair. The retractor bulbi and lateral rectus mm. are innervated by the abducent nerve (cranial nerve VI). The other three recti are innervated by the oculomotor nerve.
The dorsal oblique m. is a narrow muscle that forms a long tendon rostrally that passes through a groove in the trochlea. The trochlea is a cartilaginous plaque attached at the level of the medial angle of the eye to the wall of the orbit. This must be detached to roll the eyeball laterally. The tendon of the dorsal oblique muscle turns and courses laterally after passing around the trochlea and attaches to the sclera under the tendon of insertion of the dorsal rectus muscle. This insertion is difficult to distinguish and need not be dissected. The dorsal oblique is innervated by the trochlear nerve (cranial nerve IV).
The ventral oblique m. arises from the rostral border of the palatine bone at the level of the maxillary foramen, passes ventral to the ventral rectus, and is inserted on the sclera at the insertion of the lateral rectus. This is the only extraocular muscle that does not arise from the apex of the orbit. It is innervated by the oculomotor nerve (cranial nerve III).
To understand the action of these individual muscles, consider the eyeball as having three imaginary axes that cross in the center of the globe. The dorsal and ventral rectus muscles would rotate the eyeball around a horizontal axis through the equator from medial to lateral. The medial and lateral rectus muscles would rotate it around a vertical axis through the equator from dorsal to ventral. The oblique muscles would rotate the eyeball around a longitudinal axis passing from anterior to posterior through the center of the eyeball.
Observe: Do not try to reach the medial rectus m, more medial parts of the retractor bulbi m, nor the dorsal oblique m. Understand their location, action, and innervation. Observe all extraocular muscles that are exposed and visible from this lateral approach.
- Extrinsic muscles of the eye of the dog. A, Caudolateral aspect. (The eye is displaced slightly lateral.) B, The m. retractor bulbi, lateral aspect. 1
- Schema of motion produced by extraocular muscles. 1
- Bulbus oculi. A, Sagittal section of the dog eye with associated musculature. B, Low-magnification view of a parasagital histologic section of the canine eye. 1
- Orbit and extrinsic ocular muscles of the dog. 7
- Eye muscles
- Eye muscles
- Horse eye muscles
Bulbus Oculi (The Eyeball)
Dissect: In the following dissection, leave the bulbus oculi, or eyeball, in the orbit. The eyeball itself will not be dissected on your cadaver.
Use the eyeballs provided. The eyeballs may have attached muscles and adhered fat, which can be removed.
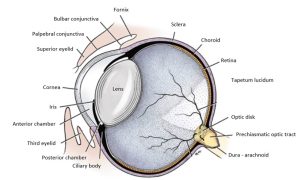
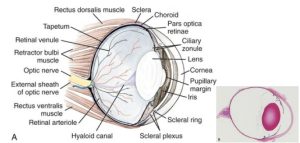
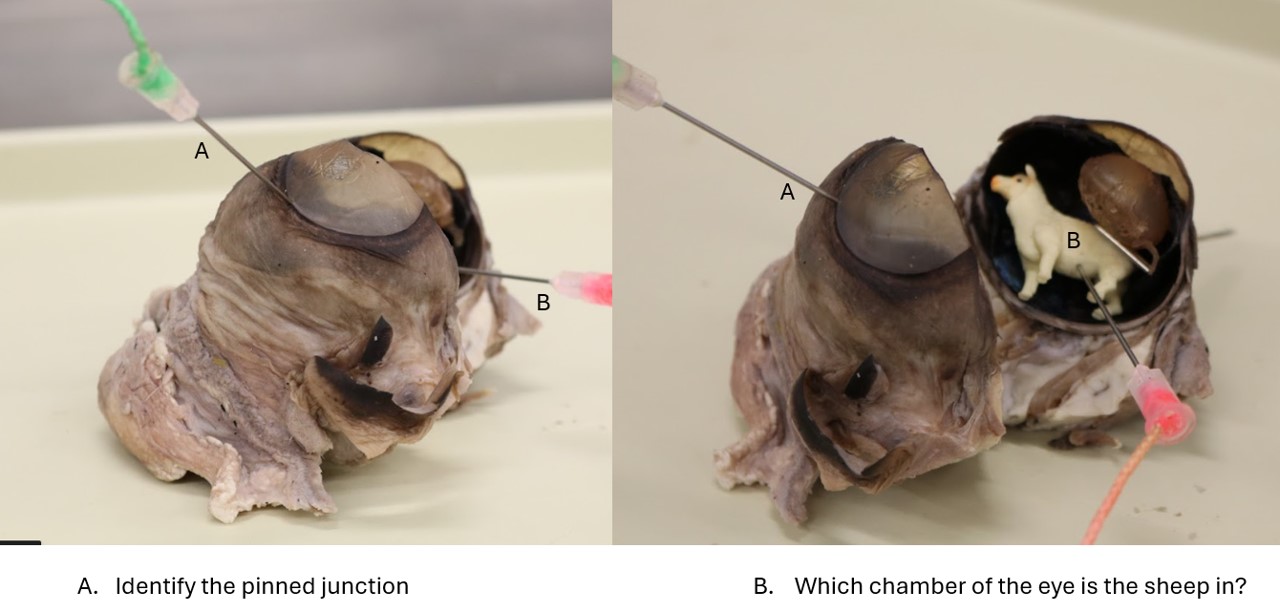
Directional terms used with reference to the eyeball are anterior and posterior and superior and inferior. The wall is composed of three layers: an external fibrous tunic, a middle vascular tunic, and an internal nervous tunic that includes the retina.
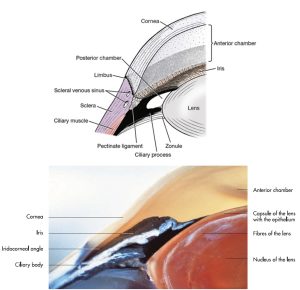
- The external fibrous tunic is composed of the cornea, which forms the anterior one fourth, and the sclera, which forms the posterior three fourths. The cornea is transparent and circular. It meets the dense, opaque sclera peripherally at the corneoscleral junction, or limbus, of the cornea. The sclera is dull gray-white. Anteriorly, it is covered by bulbar conjunctiva. Posterior to this, the extrinsic ocular muscles insert in its wall, and it is penetrated by blood vessels and nerves, including the large prechiasmatic optic tract posteriorly.
- The middle vascular tunic (the uvea) is deep to the sclera and consists of three continuous parts from posterior to anterior: the choroid, ciliary body, and iris. The iris, which has circular and radial smooth muscles, can be seen through the cornea as a pigmented diaphragm with a central opening, the pupil.
Dissect: Use a sharp scalpel to make either a sagittal cut through the eyeball from anterior to posterior pole (separating the eyeball into medial and lateral halves) or a coronal cut (separating the eyeball into anterior and posterior halves). If you were provided with dissected eyeballs (in addition to undissected eyeballs) then you should split your undissected eyeball differently (that is, if you have a dissected eyeball with a sagittal cut, then split yours coronally, or vice versa). If you were not provided with dissected eyeballs, then coordinate within your lab group to ensure that some dissection teams split eyeballs sagittally and some coronally.
Identify all of the eyeball structures listed in the terms chart above.
- Sagittal section of the eyeball of the dog. 1
- Bulbus oculi. A, Sagittal section of the dog eye with associated musculature. B, Low-magnification view of a parasagital histologic section of the canine eye. 1
- Horse eye muscles
The choroid is the posterior portion of the vascular coat and is firmly attached to the sclera. It is pigmented and lines the internal surface of the sclera as far anterior as the ciliary body posterior to the lens. The junction of the choroid and the ciliary body, called the ora serrata, is seen as an undulating line in the overlying retina. The fundus is the posterior or deep portion of the eyeball that is seen with the ophthalmoscope. The light-colored, reflective area in the dorsal part of the fundus is the tapetum lucidum of the choroid. This is a specialized layer of cells in the choroid behind the retina that reflects light rays.
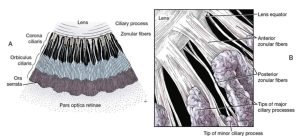
The vascular coat forms a thick circular mound at the level of the limbus. This is the ciliary body. The ciliary body, located between the iris and choroid, contains numerous muscle bundles that function in the regulation of the shape of the lens. The internal surface of the ciliary body is marked by longitudinal folds, the ciliary processes. These processes surround but do not attach to the lens at its equator. They consist of several hundred pigmented folds alternating in length, which are small at their posterior border near the ora serrata but enlarge anteriorly as they approach the lens.
The zonule is the suspensory apparatus of the lens. It is composed of numerous fine strands, zonular fibers, which pass from the region of the ora serrata along the ciliary processes to the equator of the lens. The lens is suspended from the ciliary processes by the zonular fibers. Contraction of the ciliary muscles pulls the ciliary body and processes toward the lens and therefore relaxes the tension on the zonular fibers attached to the lens. This allows the elastic lens to become more spherical and accommodate for near vision. (In other words, contraction of the ciliary muscle is required for near vision.)
The lens in an embalmed specimen is firm and opaque. In life, it is transparent and elastic. It is bounded posteriorly by the transparent jelly-like vitreous body, which fills the vitreous chamber posterior to the lens. Anteriorly, the lens is bounded by the iris and the aqueous humor. The aqueous humor fills the space between the cornea and the lens. This space is divided by the iris into two chambers. The anterior chamber is the space between the cornea and the iris. The posterior chamber is a narrow cavity between the iris and the lens. Aqueous humor is continually produced by the ciliary epithelium covering the ciliary processes. It circulates through the zonular fibers into the posterior chamber before passing through the pupil into the anterior chamber. From the anterior chamber the aqueous humor is drained through a trabecular meshwork at the iridocorneal angle, where it passes into the venous system via the venous scleral sinus. The iridocorneal angle is traversed by a meshwork of fibers with intervening spaces. This meshwork of the angle is referred to as the pectinate ligament. The integrity of this angle is critical in the drainage of aqueous humor from the eyeball. Failure in the drainage results in increased intraocular pressure, which is known as glaucoma.
Dissect: Remove the lens. Note the zonular fibers as they stretch and break.
- Section of eyeball at iridocorneal angle. 1, 7
- A, Inner surface of a ciliary body segment. B, Zonular fibers passing along ciliary processes before attaching to lens, anterior view. 1
3. The internal nervous tunic consists of the retina and its associated blood vessels and the neuronal processes surrounding the vitreous body. That portion of the retina containing the light-sensitive rods and cones, the bipolar cells, and the ganglion cells is the pars optica retinae. It covers the internal surface of the choroid from the point where the prechiasmatic optic tract enters to the level of the ciliary body. From this boundary, called the ora serrata, there is a thin non–light-receptive portion of the retina that passes anteriorly over the posterior surface of the ciliary body as the pars ciliaris retinae and continues on the posterior surface of the iris as the pars iridica retinae. The ciliary portion of the retina is two layers thick and forms the blood-aqueous barrier, through which aqueous fluid is secreted into the posterior chamber. The iridial portion of the retina is also a double cell layer consisting of pigment cells, which give the iris its color, and myoepithelial cells, which form the dilator pupillae.
In the embalmed specimen the nervous layer of the pars optica retinae has a gray-white appearance, and it readily peels away from the single layer of pigmented epithelial cells on its posterior surface, which remains attached to the choroid. This pigmented layer of the retina and the pigment of the choroid give the interior of the eyeball a brown to black appearance except where the specialized layer of the choroid, the tapetum lucidum, is located. This tapetal area exhibits a variety of brilliant colors from silver to blue to green or orange. In this area there is no pigment in the pigment epithelial cells of the retina covering the tapetum lucidum. The brown-black portion of the interior of the eyeball is sometimes referred to as the nontapetal area or nontapetal nigrum.
Observe: Notice the emergence of the prechiasmatic optic tract (aka optic nerve) from the posterior aspect of the eyeball. This is the optic disc. With careful observation of the disc, you may see the retinal vessels that enter with it to supply the internal surface of the retina.
The posterior portion of the eyeball that includes the area of the optic disc, tapetum lucidum, and adjacent uvea (nontapetal nigrum) is referred to as the fundus of the eyeball. The optic disc may be found in the interior region of the tapetum lucidum or at or below its inferior border. This varies with the breed of dog.
Review Videos & Practice
Carnivore eye structures – 5 min
Carnivore extrinsic eye muscles – 3 min
Summary of the bulbus occuli – 5 min
Horse eye structures – 25 min (covers many features noted in previous videos)
Terms
| Terms | Notes |
| External ear | |
| Pinna (auricle) | |
| Auricular cartilage | |
| Marginal cutaneous pouch | The “tick pouch” |
| External ear canal | |
| Horizontal part | |
| Vertical part | |
| Annular cartilage | |
| Tympanic membrane | |
| Eye adnexa | Adnexa [L] = “joined to” |
| Superior palpebrae | |
| Levator palpebra superioris m. | Innervated by CN III |
| Inferior palpebrae | |
| Palpebral fissure | |
| Medial/lateral palpebral commissure (canthus) | |
| Palpebral conjuctiva | |
| Bulbar conjuctiva | |
| Conjuctival fornix | |
| Conjuctival sac | |
| Third eyelid (plica semilunaris) | |
| Superficial gland of the third eyelid | Understand, don’t identify |
| Periorbita | |
| Extraocular mm. | |
| Medial rectus m. | Innervated by CN III |
| Lateral rectus m. | Innervated by CN VI |
| Dorsal rectus m. | Innervated by CN III |
| Ventral rectus m. | Innervated by CN III |
| Dorsal oblique m. | Innervated by CN IV |
| Ventral oblique m. | Innervated by CN III |
| Retractor bulbi m. | Innervated by CN VI |
| Lacrimal gland | |
| Tear drainage pathway | Understand, don’t identify |
| Dorsal/ventral lacrimal puncta → Dorsal/ventral lacrimal ducts → Lacrimal sac → Nasolacrimal duct → Rostral opening of the nasolacrimal duct | |
| Bulbus oculi | |
| Fibrous tunic | |
| Cornea | |
| Sclera | |
| Limbus | |
| Vascular tunic | |
| Iris | |
| Constrictor pupillae m. | Innervated by parasympathetic fibers of CN III |
| Dilator pupillae m. | Innervated by sympathetic fibers |
| Iridocorneal angle | |
| Lens | |
| Zonular fibers | Only present if lens remains attached |
| Ciliary body | |
| Ciliary processes | Understand, don’t identify |
| Choroid | |
| Tapetum lucidum | |
| Nervous tunic | |
| Retina | |
| Optic disc | |
| Fundus | Know what is seen during a typical fundic exam |
| Anterior chamber | |
| Aqueous humor | |
| Posterior chamber | |
| Vitreous chamber | |
| Vitreous humor |