Lab 2A: Nerves of the Thoracic Cavity
Learning Objectives
- Understand the structure and function of the autonomic nervous system.
- Identify and understand the function of somatic nerves in the thorax.
- Identify the sympathetic, parasympathetic, and somatic nn. and ganglia of the thoracic cavity.
We’ll revisit the lungs when we begin the Respiratory System unit. For now, the lungs are interfering with our ability to see the important nerves of the mediastinum, so they will need to be removed.
Dissect: Remove the left lung by transecting all structures that enter the hilus; wrap the lung in a paper towel and store it with your cadaver.
Make the transection far enough from the heart so that the vagal nerves crossing the heart are not severed but close enough so that the lobes are ideally not removed individually. Be careful of the vagus n. dorsal to the root of lung and phrenic n. ventral to the root of lung as you incise through the root of the lung.
Somatic Nerves
The motor portion of the peripheral nervous system is classified according to the type of tissue being innervated. Motor neurons supplying voluntary, striated, skeletal muscle are somatic efferent neurons. Somatic refers to the body, body wall, or head, neck, trunk, and limbs where these striated skeletal muscles are located.
Left and right phrenic nerves supply the diaphragm (a skeletal muscle, i.e. a muscle which can receive conscious control). Each nerve arises from the ventral branches of the fifth, the sixth, and usually the seventh cervical spinal nerves.
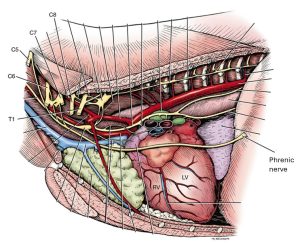
Observe: Find the phrenic nerve as it passes through the thoracic inlet. Follow the left phrenic nerve through the mediastinum to the diaphragm. If you’re having trouble finding it, the phrenic n. is the conspicuous nerve crossing the lateral surface of the heart! Identify the diaphragm as the large skeletal muscle forming the caudal boundary of the thoracic cavity.
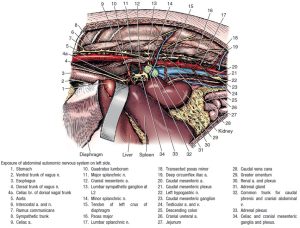
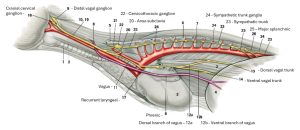
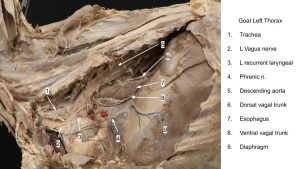
- Thoracic autonomic nerves, left lateral view, lung removed. 1
Each phrenic n. is both motor and sensory to the corresponding half of the diaphragm except at its periphery. This part of the muscle receives sensory fibers from the caudal intercostal nerves.
The recurrent laryngeal nn. carry somatic efferent fibers too. They branch from the vagus nn. and hence are discussed in detail with those nerves.
The Autonomic Nervous System
Introduction
The nervous system is highly organized both anatomically and functionally. It is composed of a central nervous system and a peripheral nervous system. The central nervous system includes the brain and the spinal cord. The peripheral nervous system comprises the cranial nerves, which connect with structures of the head and body, and the spinal nerves, which connect the spinal cord to structures of the neck, trunk, tail, and limbs. The peripheral nervous system is further classified based on anatomy and function. The nerves in this system contain axons myelinated by Schwann cells that conduct impulses to the central nervous system—sensory, afferent axons—and axons that conduct impulses from the central nervous system to muscles and glands of the body—motor, efferent axons. Most nerves have both sensory and motor axons.
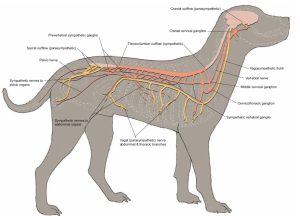
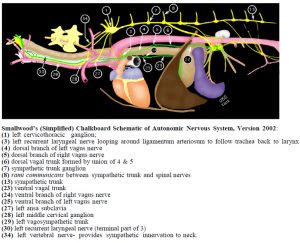
- Autonomic nervous system of the dog. 22
- Dr. Frank Mitloehner
- Dr. Frank Mitloehner
The autonomic nervous system consists of components of the peripheral and central nervous systems. Its function is to control involuntary activity, to maintain homeostasis, and to respond to stress. It differs anatomically from the somatic efferent system in having a second motor neuron interposed between the central nervous system and the innervated structures. One neuron has its cell body located in the gray matter of the central nervous system. Its axon courses in the nerves only part of the way toward the structure to be innervated. Along the course of the nerve is a gross enlargement called a ganglion (pl. ganglia). By definition, a ganglion is a collection of neuronal cell bodies located outside the central nervous system. Some ganglia have a motor function, others a sensory function. Autonomic ganglia contain the cell bodies of the second motor neurons in the pathway of the visceral efferent system. Their axons complete the pathway to the structure being innervated. Because of its relationship to the cell bodies in the autonomic ganglia, the first visceral efferent neuron with its cell body in the central nervous system is called the preganglionic neuron. The cell body of the second neuron is in an autonomic ganglion. Therefore, this neuron’s cell body is ganglionic and its axon is postganglionic.
The autonomic nervous system’s visceral efferent system is divided into two subdivisions on the basis of anatomical, pharmacological, and functional characteristics. They are the sympathetic and parasympathetic divisions. (It should be kept in mind that the autonomic nerves we observe also have visceral afferent or sensory axons within them.)

In the sympathetic division the preganglionic cell bodies are limited to the segments of the spinal cord from approximately the first thoracic to the fifth lumbar segments—the thoracolumbar portion. The cell bodies of postganglionic axons are located in ganglia that are usually only a short distance from the spinal cord. At most of the postganglionic nerve endings of this portion of the autonomic nervous system, a humoral transmitter substance, norepinephrine, is released, which causes a response in the structures innervated. The overall effect of this system is to help the body withstand unfavorable environmental conditions or conditions of stress.
In the parasympathetic division the preganglionic cell bodies are located in specific nuclei in the brain stem associated with cranial nerves III, VII, IX, and X and in the three sacral segments of the spinal cord—the craniosacral portion. The cell bodies of the postganglionic axons are often located in terminal ganglia on or in the wall of the structure being innervated. Others are found in specifically named ganglia near the innervated structure. At the postganglionic nerve endings, a humoral transmitter substance, acetylcholine, is released, which causes a response in the structures innervated. This system is associated with the normal homeostatic activity of the visceral body functions—the conservation and restoration of body resources and reserves.
The sensory (afferent) portion of the peripheral nervous system is also classified as somatic or visceral, depending on the structure innervated. Somatic afferent neurons innervate the cutaneous surface of the body, striated muscle, tendons, joints, and two specialized structures in the head: the eye and the inner ear. Visceral afferent neurons innervate the mucosal surface and wall of all tubular visceral organs, exocrine glands, and specialized vascular structures. All of these peripheral sensory neurons are single neurons between the structure innervated and the central nervous system. Their cell bodies are contained in spinal ganglia of all spinal nerves and in cranial nerve ganglia. In these ganglia there is no synapse because the synapse is in the central nervous system.
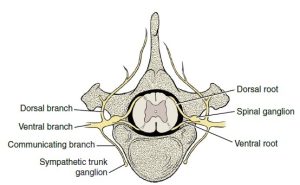
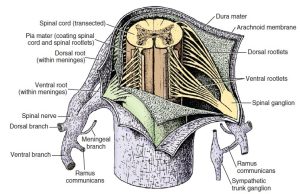
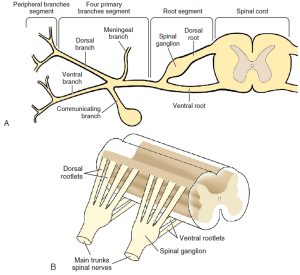
- Diagram of spinal nerve. 3
- Transected spinal cord with meninges incised to reveal a spinal cord segment, ventral view. Spinal cord roots attach to the spinal cord as a series of rootlets. Bilaterally, dorsal and ventral roots join to form a spinal nerve that immediately divides into four primary branches (dorsal, ventral, meningeal, and ramus communicans). A spinal ganglion is located on the dorsal root, and the ramus communicans joins a sympathetic trunk ganglion. 3
- A, Schematic drawing of the longitudinal segments of a typical spinal nerve. B, Schematic drawing of the dorsal and ventral rootlets of a typical spinal nerve. 3
The anatomy of the sympathetic division of the visceral efferent system requires further description before it is dissected. The cell bodies of the preganglionic neurons are located in the gray matter of the thoracic and first five lumbar spinal cord segments. Their axons leave the spinal cord along with those of other motor neurons in the ventral rootlets of each of these spinal cord segments. Each ventral root unites with the corresponding sensory dorsal root at the level of the intervertebral foramen to form the spinal nerve. The dorsal branch of the spinal nerve branches off immediately. Just beyond this point, a nerve leaves the ventral branch of the spinal nerve, the ramus communicans. It courses a short distance ventrally to join the sympathetic trunk, which runs in a craniocaudal direction just lateral to the vertebral column. A ganglion is usually located in the trunk at the point where each ramus communicans joins it. This is the sympathetic trunk ganglion and contains the cell bodies of postganglionic sympathetic axons.
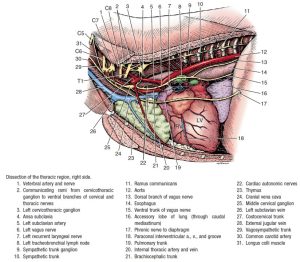
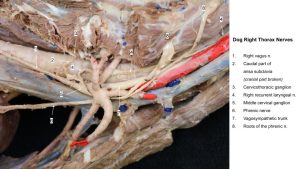
- Dissection of the thoracic region of the dog, right side. 1
- Exposure of abdominal autonomic nervous system on left side of the dog. 3
Each preganglionic sympathetic axon must pass through the ramus communicans of its spinal nerve to reach the sympathetic trunk. Its fate from here is variable and mostly dependent on the structure to be innervated.
The sympathetic trunk is located along the full length of the vertebral column on both sides. Throughout the thoracic, lumbar, and sacral levels, it is joined to each segmental spinal nerve by a ramus communicans. Only those from spinal cord segments T1 to L5 contain preganglionic axons.
Thoracic Autonomic Nervous System
Dissect: Examine the dorsal aspect of the interior of the pleural cavities. Notice the sympathetic trunks coursing longitudinally across the ventral surface of the necks of the ribs.
Dissect a portion of the trunk and a few ganglia on the left side.
The small enlargements in these trunks at each intercostal space are sympathetic trunk ganglia.
Notice the fine filaments that run dorsally between the vertebrae to join the spinal nerve of that space. These are the rami communicantes (sg. ramus communicans), of the sympathetic trunk.
- A, Schematic drawing of the longitudinal segments of a typical spinal nerve. B, Schematic drawing of the dorsal and ventral rootlets of a typical spinal nerve. 3
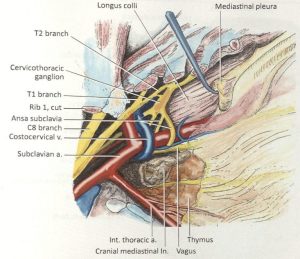
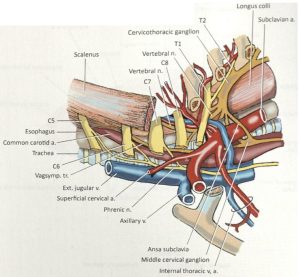
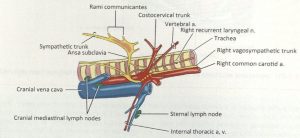
Follow the thoracic portion of the sympathetic trunk cranially. Notice the irregular enlargement of the trunk near the first intercostal space on the lateral side of the longus colli. This is the cervicothoracic ganglion. It is formed by a collection of cell bodies from a fusion of the caudal cervical ganglion and the first two or three thoracic ganglia.
Dissect: Locate the cervicothoracic ganglion on the left side by following the sympathetic trunk cranially. There is no quick way around dissecting the following structures. Carefully, bluntly dissect the nerves and separate them from the surrounding connective tissue. Before starting, take a look at the instructor dissections so you can see what the structures to be identified look like. This is time consuming and tedious work, but you can do it! Additionally, at this time you will likely find it necessary to cut and remove the first rib on the left side. Before doing so, bluntly separate any vessels or nerves that may be close to the deep surface of the first rib, so as not to damage these structures while removing the rib.
- Dissection of the thoracic region of the dog, right side. 1
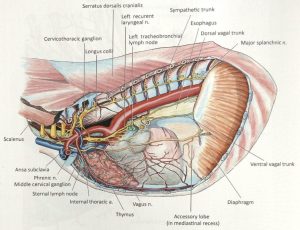
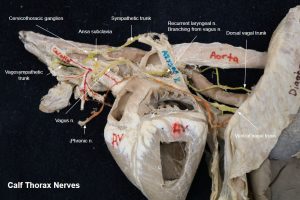
- Cranial mediastinal structures of the dog. 26
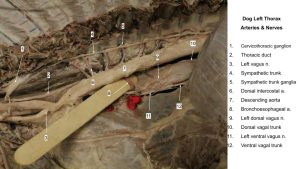
- Left mediastinum of the dog. 26
- Left cervicothoracic ganglion and associated structures of the dog. 26
- Peripheral distribution of sympathetic and parasympathetic divisions. 3
Many branches leave the cervicothoracic ganglion. Rami communicantes connect to the ventral branches of the first and second thoracic spinal nerves and to the ventral branches of the seventh and eighth cervical spinal nerves. These spinal nerves contribute to the formation of the brachial plexus, which provides a pathway for postganglionic axons to reach the thoracic limb. A branch or plexus from the cervicothoracic ganglion follows the vertebral artery through the transverse foramina. This is the vertebral nerve. This is a source of postganglionic axons for the remaining cervical spinal nerves via branches at each intervertebral space from the vertebral nerve to each cervical spinal nerve. Postganglionic axons may leave the cervicothoracic ganglion and course directly to the heart.
Dissect: Isolate and identify the vertebral n. running cranially from the cervicothoracic ganglion, and note it is closely related to the vertebral a.
- Dissection of the thoracic region of the dog, right side. 1
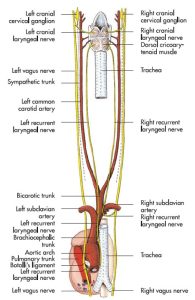
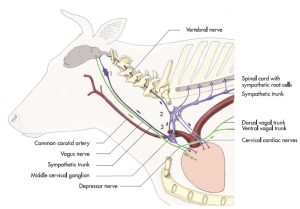
Cranial to the cervicothoracic ganglion, the sympathetic trunk divides to form a loop, the ansa subclavia, around the subclavian artery (ansa [latin], a loop-shaped structure). The two branches of the loop unite at the middle cervical ganglion. This ganglion lies at the junction of the ansa and the vagosympathetic trunk and appears as a swelling of the combined structures. Numerous branches, cardiac nerves, leave the ansa and middle cervical ganglion and course to the heart.
Dissect: Isolate and identify the ansa subclavia and middle cervical ganglion on the left side. Note that the ansa subclavia is a very delicate structure that loops around an artery (the subclavian artery).
- Dissection of the thoracic region of the dog, right side. 1
The vagosympathetic trunk in the neck lies in the carotid sheath. Its sympathetic portion carries preganglionic and postganglionic sympathetic axons cranially to structures in the head. The cranial cervical ganglion is located at its most cranial end. This is at the level of the base of the ear, just caudomedial to the tympanic bulla. It will be examined when exposed in the head dissection. The tenth cranial nerve (CN X) or vagus nerve contains parasympathetic preganglionic axons that course caudally down the neck to thoracic and abdominal organs.
Dissect: At the level of the middle cervical ganglion, notice the vagus nerve as it leaves the vagosympathetic trunk to continue its course caudally. Cardiac nerves leave the vagus n. to innervate the heart.
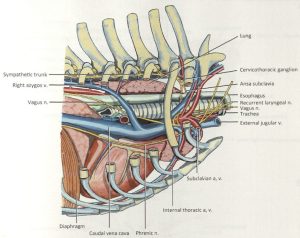
- Dissection of the thoracic region of the dog, right side. 1
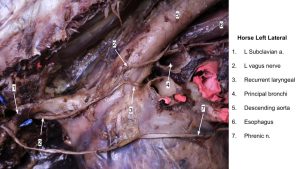
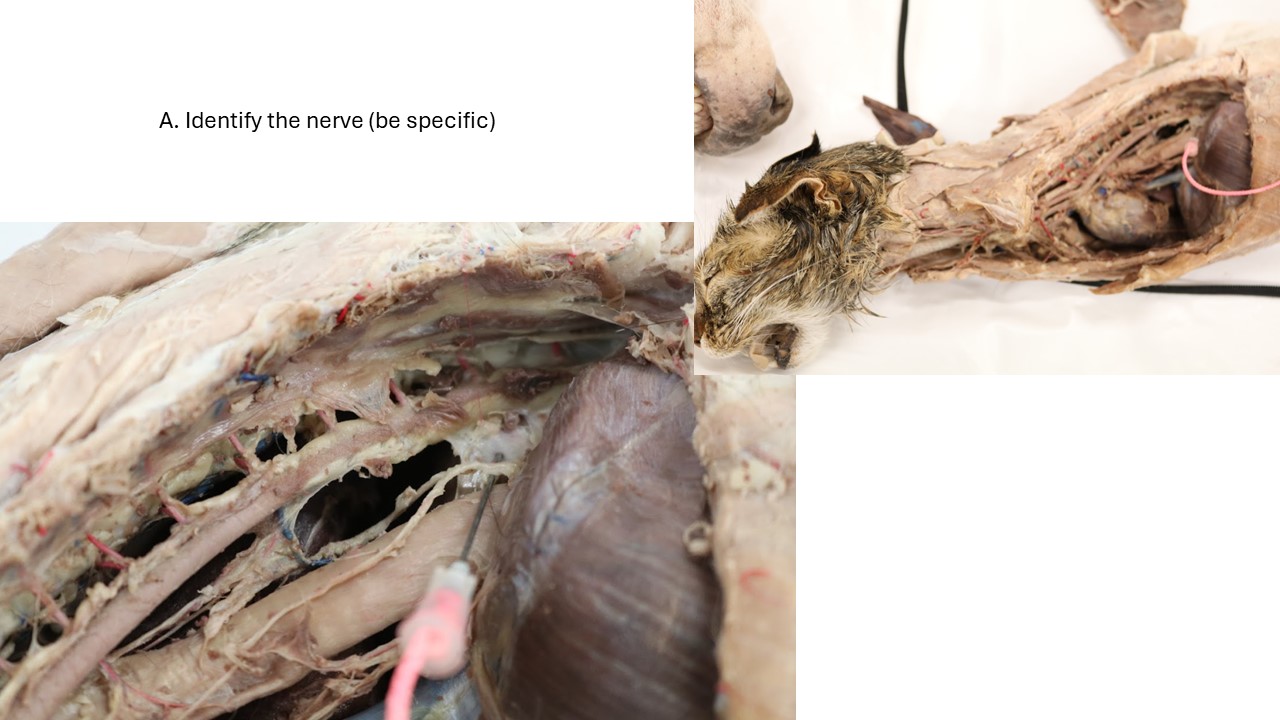
On the left side, at the level of the aortic arch, the left recurrent laryngeal nerve leaves the vagus n., curves medially around the ligamentum arteriosum (a cardiac structure which we will observe later) and the arch of the aorta and becomes related to the ventrolateral aspect of the trachea and the ventromedial edge of the esophagus. In this position it courses cranially in the neck to reach the larynx. In this course it reaches the dorsolateral aspect of the trachea.
Observe: Study the caudal course of the vagus nerve on the left side and identify the left recurrent laryngeal nerve branching off and looping around the arch of the aorta. Follow the vagus nerve as it courses over the base of the heart and supplies cardiac nerves to it.
- ANS of the neck and thorax of the cat. 4
- Illustration of the caudal (recurrent) laryngeal nerves of the horse. 7
Clinical relevance:
The left recurrent laryngeal n. exits the vagus n. at the base of the heart and passes around the aortic arch before traveling up the neck to innervate a muscle of the larynx. This pathway, and therefore the length of this left nerve, is longer than for the right recurrent laryngeal n. which exits the vagus n. cranial to the heart and wraps around the right subclavian a. before traveling up the neck.
Left recurrent laryngeal neuropathy (and subsequent left laryngeal hemiplegia) is more common than right, possibly due to the left nerve being longer.
In dogs, this nerve damage is referred to as laryngeal paralysis – often shortened to “lar par”. We will discuss this condition more in the respiratory unit.
FYI – Dogs with “lar par” – 30 seconds
On the right side, at the middle cervical ganglion, or slightly caudal to it, the right recurrent laryngeal nerve leaves the vagus n., curves craniodorsally around the right subclavian artery, reaches the dorsolateral surface of the trachea, and courses cranially to the larynx. It may be found in the angle between the trachea and the longus colli. Each recurrent laryngeal nerve sends branches to the heart, trachea, and esophagus before terminating in the laryngeal muscles as the caudal laryngeal nerve. These nerves therefore have multiple functions and carry components of the parasympathetic autonomic nervous system and general somatic efferent system.
- Illustration of the caudal (recurrent) laryngeal nerves of the horse. 7
- Structures of the right mediastinum of the dog. 26
- The right ansa subclavia and recurrent laryngeal of the dog. 26
Branches are supplied to the bronchi as the vagus passes over the roots of the lungs. Between the azygos vein and the right bronchus on the right and the area just caudal to the base of the heart on the left, each vagus n. divides into dorsal and ventral branches. The right and left ventral branches soon unite with each other to form the ventral vagal trunk on the ventral surface of the esophagus. The dorsal branches of each vagus n. do not unite until farther caudally near the diaphragm, where they form the dorsal vagal trunk, which lies dorsal to the esophagus. The termination of these trunks is found in the abdominal cavity.
Observe: Find the dorsal and ventral vagal trunks on the dorsal and ventral aspects of the esophagus, respectively. You may be able to find the dorsal and ventral branches of the left vagus nerve combining with those of the right vagus nerve to form these trunks.
- Dissection of the thoracic region of the dog, right side. 1
The Ungulate Perspective
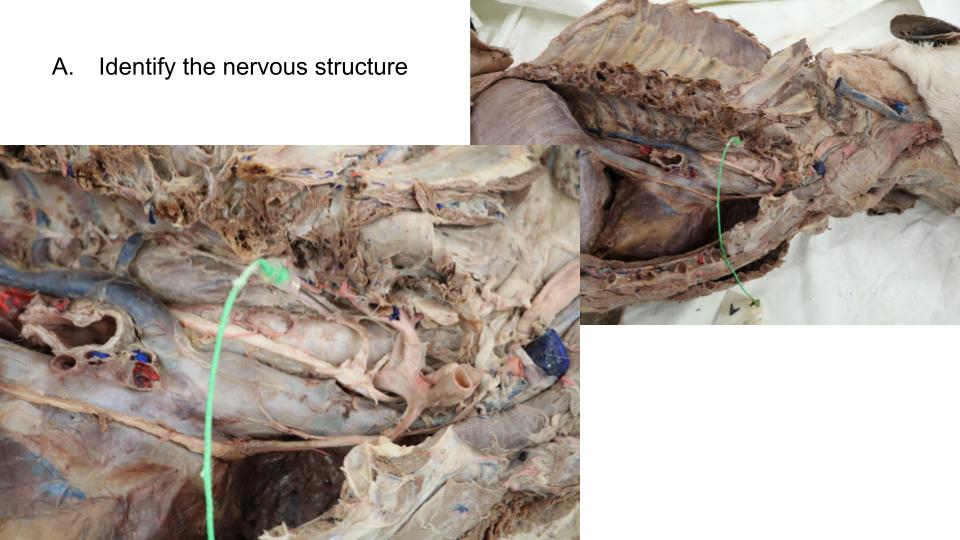
Move on to the instructors’ prosections of the ungulates to once again identify the same nerves and nervous structures described above and dissected out in your own carnivore cadavers.
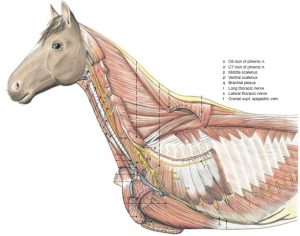
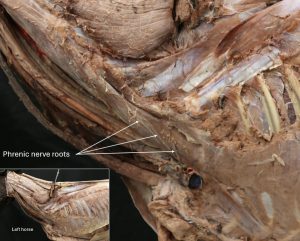
Observe: Note the stumps of the brachial plexus nerves emerging between bellies of the scalenus mm. Identify one or more intact nerves as they cross the ventral scalenus muscle – these are phrenic nerve roots, which typically arise from spinal nerves C5 to C7, with species variation.
The nerve roots combine into the phrenic n. which passes into the thorax to innervate what muscle?
- Roots of the phrenic nerve of the horse. 14
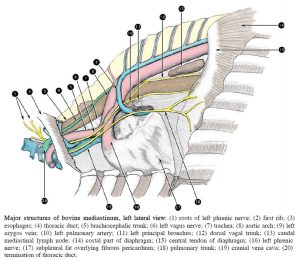
- Major structures of bovine mediastinum, left lateral view. 2
Clinical relevance:
Phrenic n. innervates the diaphragm; associated with metabolic condition in horses called Synchronous Diaphragmatic Flutter (“Thumps”), which has a characteristic respiratory pattern related to the dramatic diaphragm movements. Deep trauma in the pectoral area could damage the origin of the phrenic n.
In the pig, the left phrenic n. passes relatively close to the external jugular v. and recall we therefore prefer a right side venipuncture.
FYI – Pony with thumps – 30 seconds
Observe: Examine the internal surface of the thoracic wall to identify the intercostal neurovascular structures passing on the caudal margin of each rib. Observe a 5 cm section of this neurovascular bundle by incising the pleura on the caudal side of a rib (you should be able to spot the red and/or blue latex of the artery and vein, respectively.
Observe: Locate the vagus n., dorsal and ventral vagal branches, dorsal and ventral vagal trunks, left and right recurrent laryngeal nn., and phrenic n.
Note, only the horse’s thorax will be open on the right side, so be sure to identify these nerves on the left and right side of the horse, but only on the left side in the artiodactyls.
- 2
- Schematic illustration of the sympathetic and parasympathetic nerves in the cervical and thoracic region of the ox (1 = cranial cervical ganglion, 2 = cervicothoracic ganglion, 3 = ansa subclavia). 7
- Major structures of bovine mediastinum, left lateral view. 2
Clinical relevance:
As discussed in the carnivore section, ungulates (particularly horses) also can suffer damage to the left recurrent laryngeal nerve. Left laryngeal hemiplegia is called “roaring” in horses because of the noise made during exercise due to the inability to abduct the larynx normally. We will cover this condition more during the respiratory unit.
FYI – Horse roaring during exercise – 30 seconds
FYI – NCSU endoscopy to detect this condition – 3 min
Pathway of phrenic nn. across surface of heart is considered part of the pathogenesis behind Synchronous Diaphragmatic Flutter (aka Thumps) in the horse (phrenic nn. stimulated each time atria depolarize and contract, related to severe metabolic/electrolyte imbalances seen in competing endurance horses and colic patients for example).
Terms
Nerves of the Thoracic Cavity |
|
| Features | Species |
| Vagus n. | All |
| Left recurrent laryngeal n. | All; courses cranially to innervate cricoarytenoideus dorsalis (CAD) m. |
| Cricoarytenoideus dorsalis (CAD) m. | Understand innervation, don’t identify |
| Right recurrent laryngeal n. | Horse; Understand course, but don’t identify in the carnivore or artiodactyl |
| Dorsal and ventral brr. | Carnivores |
| Dorsal vagal trunk | All; combination of left and right dorsal brr. of vagus nn. |
| Ventral vagal trunk | All; combination of left and right ventral brr. of vagus nn. |
| Phrenic n. | All; innervates diaphragm |
| Diagphragm m. | All |
| Sympathetic trunk | Carnivores |
| Ramus communicans | Carnivores; connects sympathetic trunk ganglion to spinal nerve |
| Sympathetic trunk ganglion | Carnivores |
| Cervicothoracic ganglion | Carnivores |
| Vertebral n. | Carnivores; courses cranially from cervicothoracic ganglion |
| Middle cervical ganglion | Carnivore |
| Ansa subclavia | Carnivore |
| Subclavian artery | Ansa subclavia loops around subclavian a. |