Learning Outcomes
- Review the flow of blood through the systemic circulation (including the hepatic portal system) and the pulmonary system in the adult animal.
- Describe the location and orientation of the heart within the thoracic cavity in the domestic species.
- Define a respiratory sinus arrhythmia, and state in which species it is usually normal and when this type of arrhythmia should be of concern.
- Describe and identify the pericardial cavity and the serous and fibrous membranes of the pericardium.
- Define, and explain the indication for, a pericardiocentesis; describe where to insert a needle to perform the procedure in the the carnivore, horse, and bovine; identify this location on a skeleton.
- Name and identify the external features of the heart in situ and ex situ.
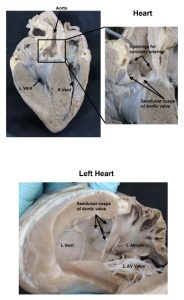
- Name and identify internal heart structures including the chambers, openings, valves, and other important features.
- Describe blood flow through the heart in adult animals.
- Identify the points of maximum intensity for auscultating the heart valves in the domestic species. Describe and identify these locations on skeletons and on cadavers.
- Explain what causes a heart murmur.
- Recognize normal heart rates, rhythms, and sounds in the domestic species and differentiate them from abnormal heart sounds.
- Name fetal heart structures of the heart and identify their remnants.
- Describe blood flow through the heart of fetal animals.
- Define a patent ductus arteriosus (PDA) and be able to differentiate the heart sounds of a normal animal from one who suffers from a PDA.
- Define the coronary arteries and their function; identify their origins in the ascending aorta.
- Identify the great cardiac vein, explain its function, and identify the coronary sinus and its opening into the right atrium.
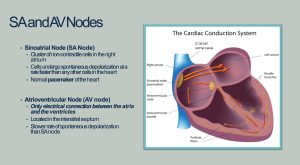
- Recall where the SA and AV nodes are located.
- Recall which heart valves are open/closed during ventricular systole and diastole.
- Recall what valves close to make the S1 and S2 heart sounds and when.
Follow these steps only when instructed to do so, depending on cadaver availability:
Dissect: We need to observe the topography of the heart in situ on both the right and left sides of the thoracic cavity while retaining the ability to study serous membranes of the thorax (pleura) undisturbed. Therefore, please pay attention to the following assignments:
The first two teams in each row of five tables will amputate the right thoracic limb and open the right thoracic cavity. In other words, one cat and one dog from each group will be opened on the right for everyone to observe. The next three tables in each group, two dogs and a cat, will be opened on the left side.
Right Side Teams: 1, 2, 6, 7, 11, 12,1 6, 17, 21, 22
Left Side Teams: 3, 4, 5, 8, 9, 10, 13, 14, 15, 18, 19, 20, 23, 24, 25
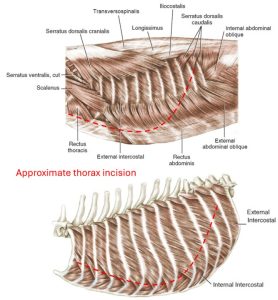
We will enter the thorax by following these directions and viewing the diagrams below:
- Skin the neck and thorax of only the side of the thorax assigned to your table. Do not skin the limb on this side. You may dispose of the skin.
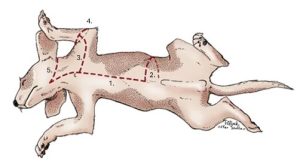
- Amputate the appropriate thoracic limb by transecting the extrinsic muscles as close to the body as possible (leave them with the limb). Do you recall all eight extrinsic muscles? Store the limb in your cadaver bag.
- Incise through rib cartilage about one inch lateral to the sternum at ribs 2-8.
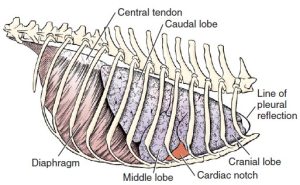
- Reach inside the thorax and feel the line of pleural reflection. Use care when doing so, as the incised ribs may be sharp. The line of pleural reflection is where the costal parietal pleura sharply turns from lining the ribs to become the diaphragmatic parietal pleura, lining the diaphragm. Basically, this is where the diaphragm is attached to the rib cage.
- Cut through the thoracic wall from ventral to caudodorsal, staying about an inch cranial to the line of pleural reflection so as not enter the abdomen.
- Reach inside the thorax and, with bone cutters, snip each rib as far dorsally as possible to reflect the wall.
- Leave rib 1 intact to avoid accidental disruption of the nn. and aa. of the cranial mediastinum. It may be removed once the dissection reaches that area.
- Video: Dr. Gerard reviews structures and the process of opening the canine left thoracic cavity – 22 minutes. Has sound.
- Video: Dr. Gerard quickly opens the canine right thoracic cavity – 5 minutes. Has basic instructions written on screen; no sound needed. Note – while he and other instructors may partially amputate the right limb, students should complete the amputation.
- Video: Lindsey opens the feline right thoracic cavity – 12 minutes. No sound needed. Filmed wearing a head mounted GoPro – occasionally shaky video.
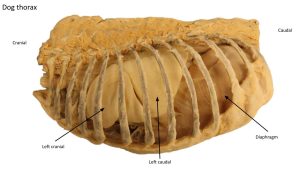
Remove the lungs by transecting all structures that enter the hilus. Make the transection far enough from the heart so that the vagal nerves crossing the heart are not severed but close enough so that the lobes are ideally not removed individually. Be careful of the vagus nn. dorsal to the root of the lung and the phrenic nn. ventral to the root of lung as you incise through the root of the lung. Keep the lung in the cadaver bag for use later. If you are working on the right side of the cadaver, be aware that the right accessory lung lobe is “tucked” into a space in between a serous membrane called the plica vena cava, which wraps around the caudal vena cava. In order to remove the right lung from the thorax, the right accessory lobe needs to be lifted dorsally and then laterally out of this space.
Blood Flow through the Adult Cardiovascular System
Observe: Most of this content is review material from lectures. Recognize that you may be assessed on these topics as they relate to laboratory content in the practical and/or written portions of assessments. Fetal cardiac circulation will be studied in this lab, and the entire system will be studied in lecture.
Adult Systemic and Pulmonary Circulation (including the hepatic portal system)
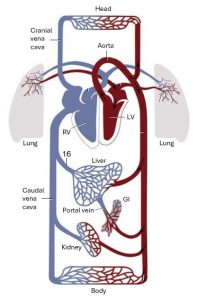
DEOXYGENATED BLOOD
Deoxygenated blood from the body returns to the heart via the cranial and caudal vena cava.
The cranial and caudal vena cava both drain into the right atrium of the heart.
Blood passes from the right atrium through the right atrioventricular (Right AV/tricuspid) valve into the right ventricle.
From the right ventricle, blood goes through the pulmonic valve into the pulmonary trunk, from which the right and left pulmonary arteries branch.
The pulmonary arteries bring blood to their respective lung lobes where carbon dioxide is replaced with oxygen.
OXYGENATED BLOOD
Oxygenated blood is carried from the lungs via the pulmonary veins into the left atrium.
From the left atrium, blood flows through the left atrioventricular (Left AV/bicuspid/mitral) valve into the left ventricle.
Blood in the left ventricle is pumped through the aortic valve into the ascending aorta and to
a. the heart muscle itself via the right and left coronary arteries, to the
b. the cranial body via branches of the aortic arch, the great vessels (brachiocephalic trunk, right and left subclavian arteries) and thoracic part of the descending aorta, including
c. to the lungs, to provide nutritional blood supply via the bronchial arteries (FYI), and
d. to the caudal body via the abdominal part of the descending aorta. Arteries then branch from the descending aorta to supply the structures of the abdomen, pelvic cavity, and pelvic limbs.
-
Schematic drawing of the systemic and pulmonary
circulation. 8
DEOXYGENATED blood returns to the cranial and caudal vena cava by one of several routes:
a. from the caudal body via the azygous vein(s) to the cranial vena cava;
b. from the head and neck veins into the cranial vena cava;
c. from the lungs via bronchial veins (FYI);
c. from peripheral veins which drain directly into the caudal vena cava; or
d. via the hepatic portal system (a subpart of the systemic circulation) whereby blood pumped from the gastrointestinal track passes through the hepatic portal vein to the liver, where digestive toxins are removed, and then through the hepatic vein to the caudal vena cava. Note that the hepatic portal vein (often just called portal vein) and the hepatic vein are very different structures, which carry blood to and from the liver, respectively. Also note that the liver receives both oxygenated (nutritional) and deoxygenated (functional) blood from branches of the descending aorta and portal system respectively.
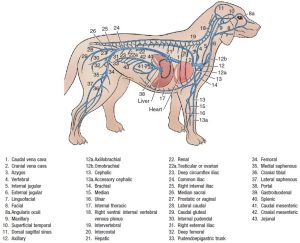
- Schema of the venous system 1
Practice: Can you start anywhere in the circulation and describe the travel of a red blood cell from that starting place? Do you know which vessels are carrying deoxygenated vs. oxygenated blood?
Heart and Pericardium
In this section, the heart will be studied in situ (in place) in the cadavers of all species, as well as using the wet and dry specimens to learn the external and internal features and structures of the heart. A cadaveric porcine heart will be provided for dissection. The anatomy of the heart itself is relatively constant among domestic mammals and so will be studied at the same time for small and large animals. The location and orientation of the heart is similar among species as well, and you are responsible for identifying the external structures in situ and ex situ. The great vessels branch differently among species. These differences will be discussed in the vasculature of the thorax, later in this unit.
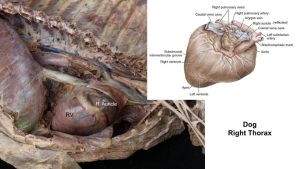
Heart Topography
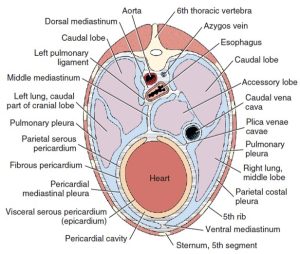
The heart is the muscular pump of the cardiovascular system. The musculature and conducting system of the heart are spoken of collectively as the myocardium. The heart is cone-shaped and obliquely placed in the thorax so that its base faces dorsocranially and its apex is directed ventrocaudally and to the left side. A small, roughly triangular area of its dorsocaudal surface adjacent to the apex is related to the diaphragm. The large remaining part of its circumference is largely covered by the lungs and faces the sternum and ribs.
The heart is located in the middle part of the mediastinum, the partition that separates the two pleural cavities. It is the largest organ in this tissue-filled septum located between the two pleural cavities. Covered by its pericardium, the canine heart extends from the third rib to the caudal border of the sixth rib in the canine.
- The feline heart is located relatively more caudally in the thorax. It extends from the 4th intercostal space (ICS) to the level of the 7th rib.
- Schematic transverse section of the thorax. 1
- Left and right surface projections of the feline heart. 8
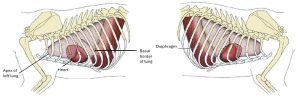
- Thoracic cage and lungs of the dog. Right side. 1
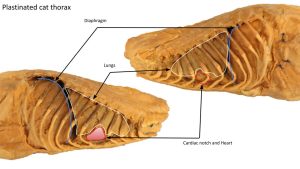
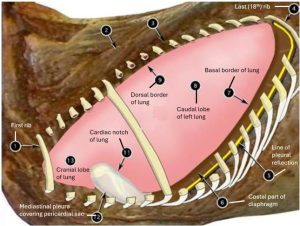
In the carnivore, the cardiac notch of the right lung is a V-shaped area formed by the ventrally diverging borders of the cranial and middle lobes. On the left side usually no obvious cardiac notch is formed. The ungulate species possess a cardiac notch on both sides of the thorax. This anatomy becomes relevant when performing a pericardiocentesis, which is a procedure we will discuss later in this chapter.
Observe: Observe the left heart structures in student cadavers. Observe prosections of the carnivore right thorax, when provided. Observe left and right sides on ungulate cadavers. Note where the structures are located within the thoracic cavity. Replace the lung on the right side of a carnivore and observe the cardiac notch.
Clinical Application: Heart Auscultation Part 1; Normal Heart Sounds

Listening to the heart sounds on both the left and right sides of patients is an imperative part of any physical examination. When listening to the heart, we are assessing 1. the rate of the heart beat, 2. the rhythm of the heart beat, and 3 and 4. normal and abnormal sounds made by valve closures and the flow of blood through the heart.
The normal dog and cat have two heart sounds, S1 and S2. Healthy horses can have up to four heart sounds! The normal heart rate can vary considerably. In dogs, a low resting heart rate is normally associated with a slight increase in the rate during inspiration and a decrease during expiration. This normal phenomenon is called a respiratory sinus arrhythmia. Cats usually do not have respiratory sinus arrhythmia, and if present, it should raise the suspicion of respiratory disease.
REQUIRED: If you have not done so yet, take a moment to join VIN here. Then listen to the following audio recordings of normal heart sounds. You will be tested on recognizing a normal vs. abnormal heart beat in dogs, cats, and horses.
LISTEN: Normal Canine Cardiac Rhythm
LISTEN: Normal equine heart sounds (soundtrack #’s: 43-48)
LISTEN: Normal feline heart sounds (focus on soundtrack 5 for now).
Observe: As the external features and chambers of the heart are described below, make sure to note where these structures are in situ, on the right and left sides, as well as ex situ. You are responsible for identifying the four chambers and external feature of the hearts in both scenarios. On both the left and right sides, be able to state and identify where the heart is located on a skeleton of each species.
Pericardium
The pleurae are serous membranes that cover the lungs and line the walls of the thorax. These form separate right and left sacs that enclose the pleural cavities (i.e. there is one thoracic cavity with a left and right pleural cavity contained within). Between the pleural cavities, on midline, is the mediastinum. The pleura will be studied more in depth during the respiratory unit. For now, understand that the mediastinum is a space on the midline of the thoracic cavity wherein the heart, trachea, and esophagus, among other structures, are located. The heart is located in the middle part of the mediastinum from the level of the third to the sixth rib. This space is bordered on either side by a very thin serous membrane called the mediastinal pleura. The specific part of the mediastinal pleura over the heart is further classified as pericardial mediastinal pleura.
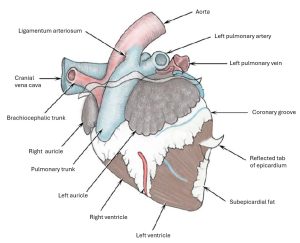
The pericardium is the fibroserous covering of the heart. It is a thin but strong layer consisting of three inseparable components: the outer pericardial mediastinal pleura (see above), a middle fibrous pericardium, and an inner parietal pericardium. The continuation of the fibrous pericardium to the sternum and diaphragm forms the phrenicopericardial ligament. This is located in the ventral mediastinum along with a variable amount of fat. The parietal pericardium is a closed sac that envelops most of the heart. The parietal layer adheres to the inside surface of the fibrous pericardium. At the base of the heart it is continuous with the visceral pericardium (epicardium), which tightly adheres to the heart. Between the parietal and visceral pericardia is the pericardial cavity, which contains a small amount of pericardial fluid.
Dissect: On the in situ hearts, incise and reflect the pericardium, consisting of its three layers, 1. the very thin pericardial mediastinal pleura (often has fat incorporated), 2. the fibrous pericardium, and 3. the parietal pericardium to expose the pericardial cavity and the heart surface. The surface of the heart is covered with the visceral pericardium or epicardium. The heart muscle itself is the myocardium. Most of the time, the pericardium will have been removed from the ex situ hearts, but if not, you may observe these tissue layers on them as well.
Clinical Application: Pericardial Effusion and Pericardiocentesis
Pericardial effusion refers to a condition in which fluid, usually blood, accumulates in the pericardial cavity, constricting the heart and ultimately affecting cardiac function. The heart sounds will be extremely muffled due to the fluid. Depending on the severity of the condition, patients will usually present in some level of respiratory distress and/or with increased capillary refill time (the time it takes gingiva (gums) to turn pink again after pressing on them), because the the heart is not able to pump properly, the output is severely decreased, and the patient becomes hypoxic (low oxygen). Treatment for this condition is a pericardiocentesis whereby a needle is passed into the pericardial cavity in order to drain the fluid.
Q: In what intercostal space, and on what side of the patient, would you perform a pericardiocentesis in a dog? And in a cat? Why?
READ MORE: canine pericardial effusion


Severe pericardial effusion in a dog, dorsoventral projection (Photo by Dr. Mark D. Kittleson). Right lateral radiograph of dog with pericardial effusion. These images are not from the same patient.


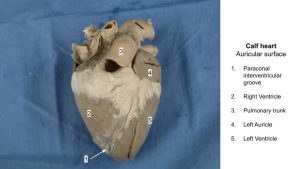
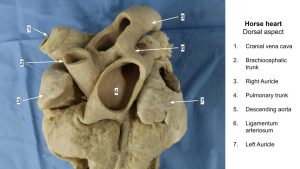
Observe: Observe the following bolded external features/structures of the heart as you read the passage below. Be sure to identify them ex situ and on both sides of the thorax in situ, where applicable.
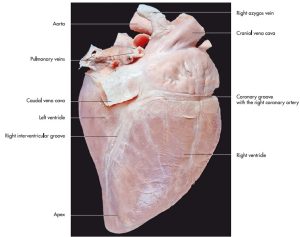
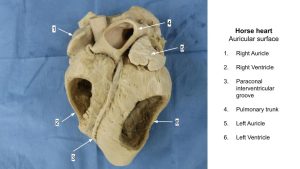
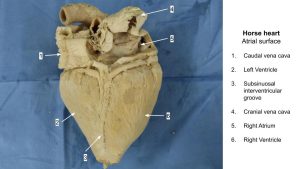
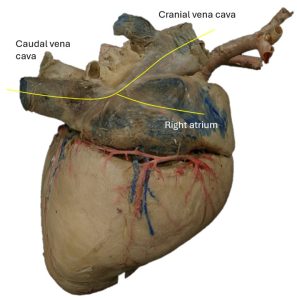
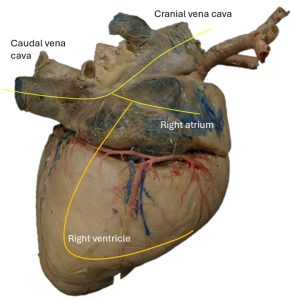
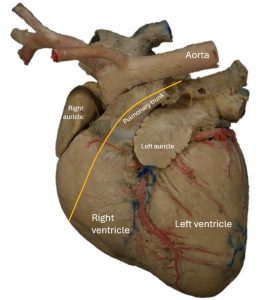
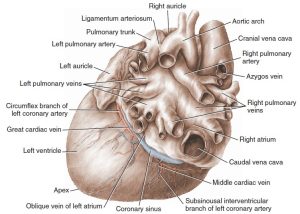
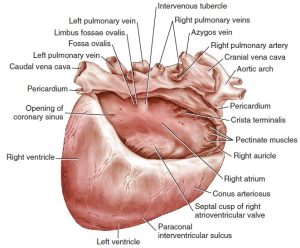
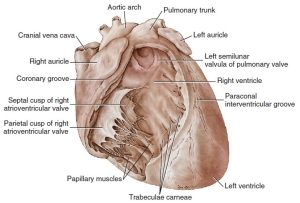
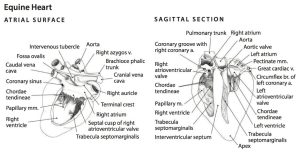
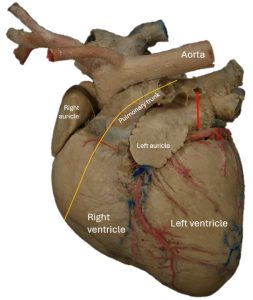
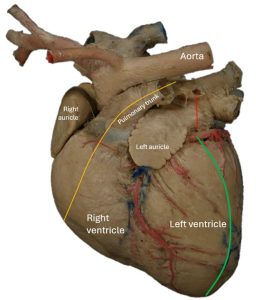
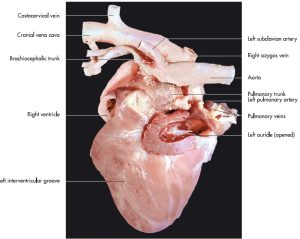
External heart
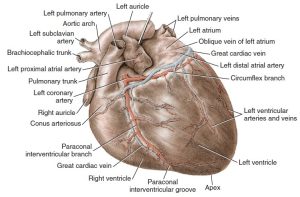
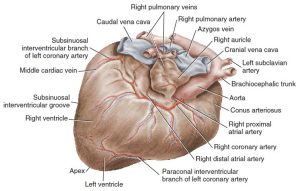
The heart consists of a dorsal base, where the great vessels are attached, and an apex that faces ventrally, caudally, and usually to the left, depending on the shape of the thorax. The surface of the heart facing the left thoracic wall is called the auricular surface because the tips of the two auricles project on this side. The auricles are small appendages of each atrium. The opposite surface facing the right thoracic wall is the atrial surface. The thin-walled right ventricle winds across the cranial surface from the atrial surface of the heart; it can be observed on the right and left sides of the thoracic cavity. Likewise, the left ventricle winds around the caudal surface of the heart and may be observed on both sides of the thorax.
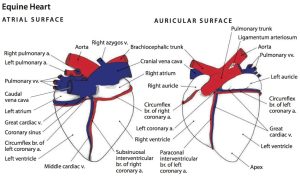
The coronary groove lies between the atria and ventricles and contains the coronary vessels and fat. The interventricular grooves are the superficial separations of the right and left ventricles. They represent the approximate position of the oblique interventricular septum. Obliquely traversing the auricular surface of the heart is the paraconal interventricular groove. It begins at the base of the pulmonary trunk, where it is covered by the left auricle. Note that the paraconal interventricular groove is adjacent to the conus arteriosus (FYI), which is the outflow tract of the right ventricle. FYI: This groove contains the paraconal interventricular branch of the left coronary artery. The shorter and less distinct subsinuosal interventricular groove lies on the caudal aspect of the atrial surface ventral to the level of the coronary sinus (subsinuosal) that enters the right atrium. FYI: This groove contains the terminal branch of the left coronary artery.
Observe: Trace the coronary groove around the heart. Note that this groove separates the atria from the ventricles and that it contains coronary vessels and fat, which supply the heart muscle itself. Identify the base and apex of the heart, the auricular and atrial surfaces, and the interventricular grooves. Do so in situ and ex situ.
- The heart, auricular surface. 1
- The heart, atrial surface. 1
- Heart of a newborn calf; left lateral view. 2
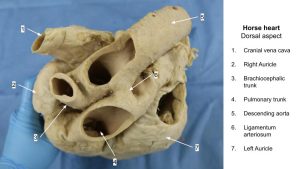
- External structures and vessels of the horse heart, atrial and auricular surfaces. 6
- Heart of a horse (atrial surface). 7
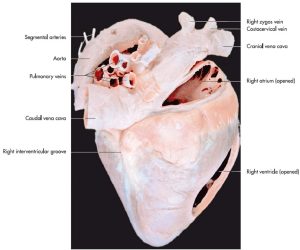
- Heart of a horse (atrial face). 7
- Heart of a horse (atrial face).
Clinical Application: Heart Auscultation Part 2: Cardiac Arrhythmias
Cardiac arrhythmias occur when electrical impulses in the heart don’t work properly and the heart beats too fast, too slowly, and/or irregularly. We can hear this irregularity, and clinicians may use an electrocardiogram (ECG, also called an EKG) and/or phonocardiography to confirm and further elucidate specific types and causes of arrhythmias. Listen to the arrhythmias linked below. You need not know what kind each is, but for our purposes, be able to differentiate these from normal heart rhythms (see heart auscultation part 1). Note you must have activated your free student VIN membership to listen to these examples.
LISTEN: Carnivore arrhythmias
LISTEN: Equine arrhythmias
Internal Heart Dissection
- Identify the atrial surface (right side) of the heart.
Ways to identify the right side:
-
-
- The apex of the heart will be pointed caudally. Use this fact to orient yourself.
- If the descending aorta is still on the specimen, it will always be coursing caudally.
- Identify the left and right auricles, which will be observed on the auricular (left) side.
-
- Locate the cranial and caudal vena cava and right atrium. In situ, the caudal vena cava will be observed on the right side of the thorax. Do not worry about dissecting out the cranial vena cava in your cadavers, but know where it is located.
Dissect:
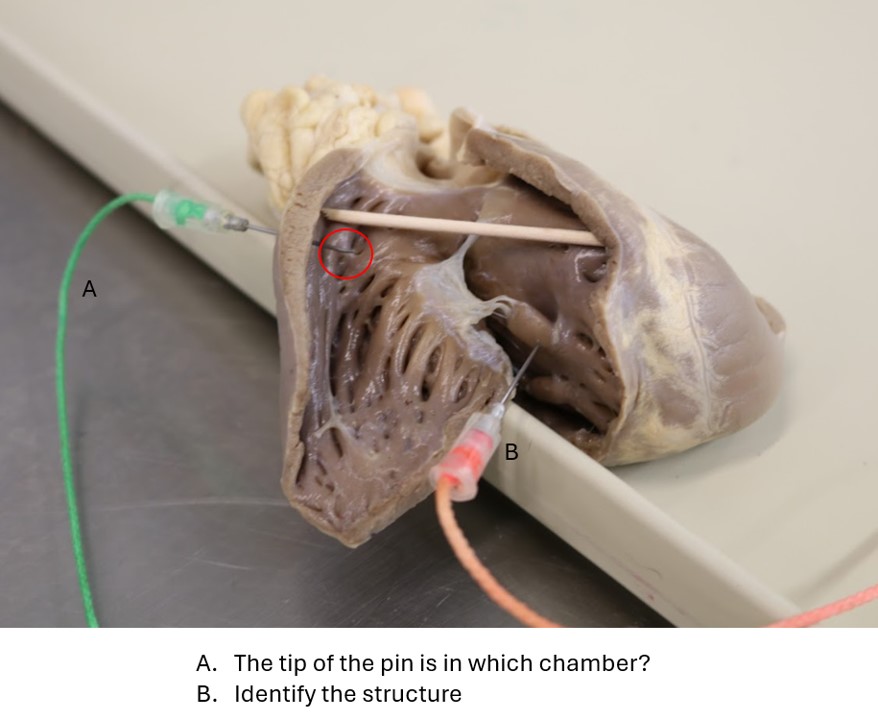
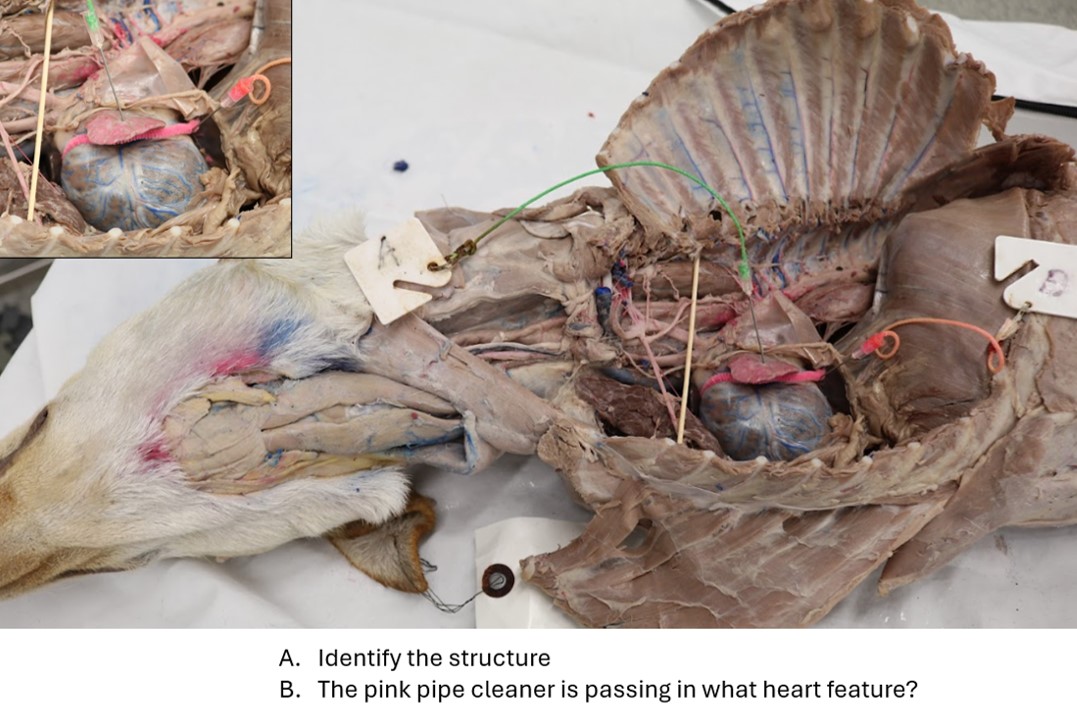
- Make an incision along the length of the vena cava and into the right atrium, as in the photograph below.
- Extend the incision into the right atrium, through the right AV valve, and into the right ventricle.
- Continue the incision and make a U-shaped cut into the right ventricle, exiting through the pulmonary artery.
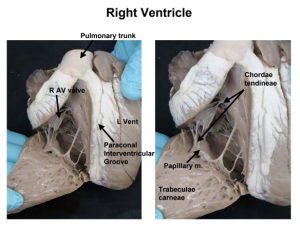
Observe: Observe the following bolded internal cardiac structures. Recall where the SA and AV nodes are located.
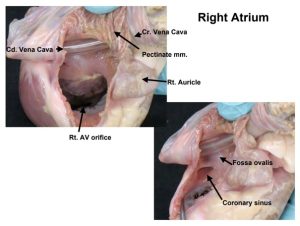
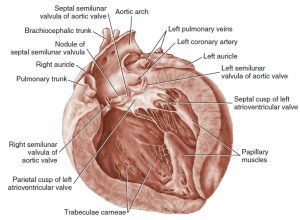
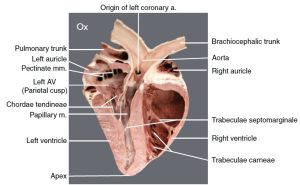
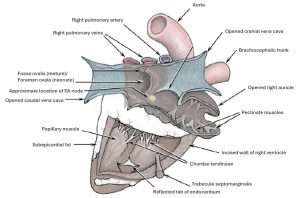
The right atrium receives the blood from the systemic veins and most of the blood from the heart itself. It lies dorsocranial to the right ventricle. Recall that the SA node is located within the wall of the right atrium. It is divided into a main part, the sinus venarum, and a blind cranial part, the right auricle.
There are four openings into the sinus venarum of the right atrium. The caudal vena cava enters the right atrium caudally. Ventral to this opening is the coronary sinus, the enlarged venous return for most of the blood from the heart. The subsinuosal interventricular groove is ventral to this sinus on the atrial surface of the heart. The cranial vena cava enters the atrium dorsally and cranially. Ventral and cranial to the coronary sinus is the large opening from the right atrium to the right ventricle, the right atrioventricular orifice. The valve will be described with the right ventricle.
Examine the dorsomedial wall of the sinus venarum, called the interatrial septum, which separates the left and right atria. Recall that the AV node is located within the interatrial septum.
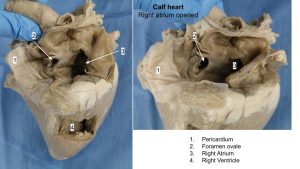
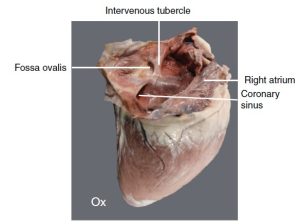
Between the two caval openings is a transverse ridge of tissue, the intervenous tubercle (FYI). It diverts the inflowing blood from the two caval veins toward the right atrioventricular orifice. Caudal to the intervenous tubercle is a slitlike depression, the fossa ovalis. In the fetus there is an opening at the site of the fossa, the foramen ovale, which allows blood to pass from the right to the left atrium, thereby bypassing the developing lungs.
Observe: Observe the fossa ovalis on mature hearts.
- The heart, atrial surface. 1
- External structures and vessels of the horse heart, atrial and auricular surfaces. 6
- Heart of a horse (atrial surface). 7
- Heart of a horse (atrial face). 7
- Heart of a horse (atrial face).
- Fossa ovalis
Locate the pulmonary trunk leaving the right ventricle at the left craniodorsal angle of the heart.
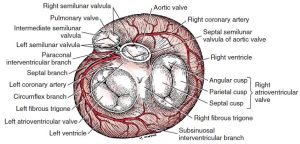
The greater part of the base of the right ventricle communicates with the right atrium through the atrioventricular orifice. This opening contains the right atrioventricular valve. This valve is also commonly called the right AV valve, or the tricuspid valve. You must be able to use these terms interchangeably.
There are two main parts to the valve in the dog: a wide but short flap that arises from the parietal margin of the orifice, the parietal cusp, and a flap from the septal margin, the septal cusp, which is nearly as wide as it is long. Subsidiary leaflets are found at each end of the septal flap. The points of the flaps of the valve are anchored to the septal wall of the ventricle by the chordae tendineae. The chordae tendineae are attached to the septal wall by means of conical muscular projections, the papillary muscles, of which there are usually three to four.
The trabeculae carneae are the muscular irregularities of the interior of the ventricular walls. The trabecula septomarginalis is a muscular strand that extends across the lumen of the right ventricle from the septal to the parietal wall (the parietal wall being the ‘outer margin’ of the ventricle). The septal attachment is often to a papillary muscle. The trabecula septomarginalis serves for the passage of cardiac conduction fibers from the right branch of the atrioventricular bundle across the lumen of the cavity.
The right ventricle passes across the cranial surface of the heart and terminates as the funnel-shaped conus arteriosus, which gives rise to the pulmonary trunk. This is at the left craniodorsal aspect of the heart. Recall that the paraconal interventricular groove is adjacent to the caudal border of the conus arteriosus on the auricular surface of the heart.
At the junction between the right ventricle and the pulmonary trunk is the pulmonary valve, which consists of three semilunar cusps. A small fibrous nodule is located at the middle of the free edge of each cusp. The pulmonary trunk bifurcates into right and left pulmonary arteries, each going to its respective lung.
- The heart, dorsal aspect. 1
- The interior of the right atrium. 1
- Interior of the right ventricle, ventral aspect. 1
- Internal structures of the horse heart, atrial view with right atrium and ventricle exposed and sagittal section with all chambers exposed. 6
- Tricuspid valve
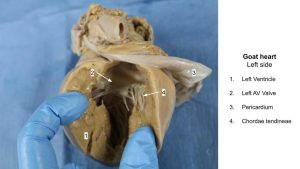
Dissect:
- Rotate the heart to find the left atrium and ventricle.
- Cut through one of the pulmonary veins down into the left atrium and observe the left atrioventricular valve.
- After observing the left AV valve, continue cutting down through the valve, into the left ventricle.
- Enter the cut end of the aorta and incise to the aortic valve without cutting through the valve itself. Observe the bolded structures below as you read their descriptions.
The left atrium is situated on the left dorsocaudal part of the base of the heart dorsal to the left ventricle. Five or six openings mark the entrance of the pulmonary veins into the atrium. The inner surface of the atrium is smooth except for pectinate muscles confined to the left auricle. The interatrial septal wall separates the left and right atria.
Notice the thickness of the left ventricular wall as compared with the right. Why the difference?
The left atrioventricular valve is composed of two major cusps, the septal and parietal, but the division is indistinct. Secondary cusps are present at the ends of the two major ones. The left atrioventricular (AV) valve is also called the bicuspid valve or mitral valve. You must be able to use these terms interchangeably.
Notice the two large papillary muscles and their chordae tendineae attached to the cusps.
The aortic valve, like the pulmonary valve, consists of three semilunar cusps. Behind each cusp, the aorta is slightly expanded to form the sinus of the aorta.
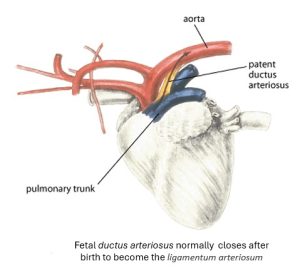
A fibrous connection, the ligamentum arteriosum, is located between the pulmonary trunk and aortic arch, just caudal to the left subclavian a. In the fetus it was the patent ductus arteriosus and served to shunt blood from the right ventricle directly into the descending aorta, thereby bypassing the nonfunctional lungs.
Observe: On the external surface of a mature heart specimen, identify the ligamentum arteriosum. Identify and carefully pass a probe through the ductus arteriosus on a neonatal calf heart (wet specimen). Observe the ductus arteriosus on the left side of the instructor calf cadaver.
- The heart, auricular surface. 1
- Interior of the left ventricle, left lateral aspect. 1
- External structures and vessels of the horse heart, atrial and auricular surfaces. 6
- Internal structures of the horse heart, atrial view with right atrium and ventricle exposed and sagittal section with all chambers exposed. 6
- Heart of a dog (auricular surface). 7
- Bovine heart, sagittal section. 12
Recall that ventricular systole is when the left and right ventricles contract. Blood pressure within the ventricles increases dramatically, forcing blood through the semilunar valves (aortic and pulmonic), which are opened due to this blood flow. This same increased pressure closes the AV valves, which causes the S1 heart sound.
Ventricular diastole occurs when the heart muscle relaxes. Blood pressure in the emptied ventricles decreases. Blood in the aorta and pulmonary trunk closes the semilunar valves, causing the S2 heart sound, and blood flows into the atria and through the AV valves, which the blood flowing into the ventricles has forced open.
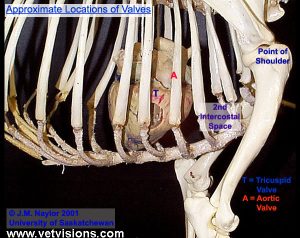
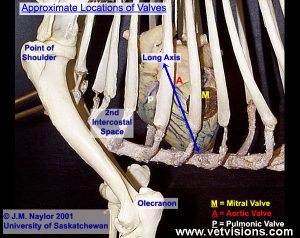
Clinical Application: Points of Maximum Intensity
Each of the heart valves can best be heard at a specific location on the patient. These locations are called points of maximum intensity and are as follows. Be able to identify these locations on a heart in situ, on skeletons, and on the exterior surface of a patient:
Heart valve points of maximum intensity for the dog and cat:
Mitral/bicuspid/Left AV = Left 5th intercostal space, a bit ventral to the shoulder joint
Aortic = Left 4th intercostal space, a bit more dorsally than mitral.
Pulmonic = Left 3rd intercostal space, at costochondral junction
Tricuspid/R AV: RIGHT 4th intercostal
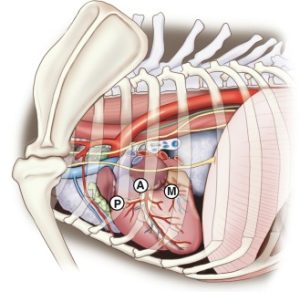
- Right lateral view of the canine thorax. M – mitral, A – aortic, P – pulmonic. 9
- External diagram of PMI’s Ilaria Spalla
The heart valve points of maximum intensity for the equine patient are:
Pulmonic valve = left, low 3rd intercostal space (ICS)
Aortic valve = left, higher 4th ICS
Mitral (LAV) = left, lower 5th ICS
Tricuspid (RAV) = right, low 3rd or 4th ICS
Heart Valve Point of Maximum Intensity (PMI) for the bovine patient:
Same as the horse except for the Mitral (LAV) which is on the left, lower 4th ICS.
Mnemonics: PAM345LHL (horse) and PAM344LHL (ox); and RAV3.4L for tricuspid valve (a “Toyota RAV 3.4L”!?).
-OR- MAP543 for the horse, dog, and cat.
Note that one has to shift the thoracic limb cranially to access ICSs for the pulmonary and tricuspid valves and that the triceps muscle mass covers the cranial thorax.
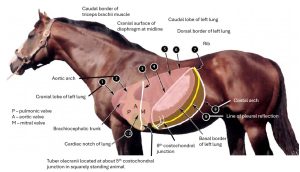
- Projections of selected thoracic viscera onto body surface of horse. 2
- Left horse thorax. 2
Clinical Application: Heart Murmurs
Heart murmurs are caused by turbulent blood flow in the heart. They are often indicative of a structural abnormality, but not always. Defects of the valves are best heard at the points of maximum intensity, which is why it is important to listen to heart sounds at all of these locations.
-
FYI: The most common congenital cardiac defects of dogs are patent ductus arteriosus (see below), pulmonic stenosis (abnormal narrowing), and aortic stenosis.
-
FYI: The most common congenital cardiac defects of cats are atrioventricular septal defects and atrioventricular valve dysplasia.
The presence of a loud systolic murmur, or any diastolic or continuous murmur is supportive of congenital heart disease and warrants further investigation. Congenital heart defects range in severity and complexity, and early detection and treatment may improve the outcome with certain conditions.
The presence of a heart murmur in a young animal is not pathognomonic for a congenital heart defect. Many young animals will have a low-grade systolic murmur (often grade II/VI or less) that is “innocent” and caused by mild turbulence that is not associated with a congenital heart defect. These murmurs usually disappear by 6 months of age in dogs and cats.
****Be able to differentiate between normal and abnormal heart sounds in a dog, cat, and a horse.****
LEARN MORE: Common Congenital Cardiovascular Defects in Domestic Livestock (FYI)
LISTEN: Carnivore Murmurs
LISTEN: Normal Equine Heart Murmurs
LISTEN: Abnormal Equine Heart Murmurs
READ MORE:
Congenital and Inherited Anomalies of the Cardiovascular System in Animals
By
Neonatal structures of the Calf Heart
Fetal Circulation
Because the lungs are essentially non-functional while in utero, fetal circulation varies from adult circulation via its primary oxygenated blood source, the placenta. Fetal circulation through the heart has two main routes: the first is blood flow from the right atrium directly to the left atrium via an opening called the foramen ovale. This serves to shunt highly oxygenated blood coming from the placenta directly to the left side of the heart for distribution to systemic circulation. The second main route is through the ductus arteriosus, a small communication between the pulmonary artery (PA) and the aorta (Ao). In the fetus, PA pressure is higher than Ao pressure, so blood flows from the PA through the ductus into the Ao. Although these routes bypass the lungs, a small amount of blood flows via the normal adult pathway which bathes the developing pulmonary tissues with oxygen and nutrients.
After parturition, when the lungs become functional tissue and the placenta is removed from fetal circulation, pulmonary vascular resistance drops and systemic vascular resistance increases. These pressure changes drive the circulation that occurs in adults: the left side of the heart and systemic circulation become the high-pressure system, while the right side of the heart and the pulmonic circulation become the lower-pressure system. The ductus arteriosus closes when highly oxygenated blood from the lungs reaches its baroreceptors, about 24–48 hours after parturition.2 Additionally, the increased pressure and volume on the left side of the heart functionally closes the foramen ovale, ceasing communication between the two atria. In the first few weeks of life, cardiac development finishes as the left ventricle reaches the thickness in which it remains for the rest of the animal’s life.3
[See WVC Conference 2024 proceedings for full citations, linked here via VIN (REMEMBER TO JOIN!!) ]
Observe: Review the ductus arteriosus (left side) and foramen ovale (right side) of the calf hearts, in situ. Also observe these structures in calf hearts ex situ. Differentiate these structures from the analogous structures in the adult.
- Heart of a newborn calf; left lateral view. 2
- Heart of a newborn calf; right lateral view with right atrium and ventricle opened.2
- Bovine heart. Right atrium opened to show interior structures. 12
Clinical Application: Patent Ductus Arteriosus
Patent ductus arteriosus (PDA) is a common congenital defect of dogs, and it occurs less commonly in cats. Persistent flow through the ductus leads to excess blood flow (volume overload) to the pulmonary circulation and left heart chambers, most commonly leading to left CHF within the first 1–2 years of life. PDA occurs most commonly in small-breed dogs and causes a continuous murmur loudest over the left base and bounding pulses. Prompt diagnosis and treatment (either by interventional device occlusion or surgical ligation) before the development of clinical signs is associated with an excellent outcome. Merck Veterinary Manual.
Listen to the heart sounds of dogs with a patent ductus arteriosus (here and here). You likely have to download the files and have either Quick Time Player (Mac) or Windows Media Player installed in order to listen to these.
Another example: Patent ductus arteriosus
- Patent ductus arteriosus viewed from the left.
- The base of the heart; atrioventricular, aortic, and pulmonary valves, craniodorsal aspect. 1
Coronary vessels
The right and left coronary arteries branch from the ascending aorta and supply the heart muscle itself with oxygenated blood. The coronary veins carry deoxygenated blood from the heart muscle to the right atrium.
The right coronary artery leaves the right sinus of the aorta. It encircles the right side of the heart in the coronary groove and FYI: often extends to the subsinuosal interventricular groove. It sends many small and one or two large descending branches over the surface of the right ventricle.
The left coronary artery is about twice as large as the right. It is a short trunk that leaves the left sinus and immediately terminates in FYI: (1) a circumflex branch, which extends caudally in the left part of the coronary groove and supplies the subsinuosal interventricular branch, and (2) a paraconal interventricular branch, which obliquely crosses the auricular surface of the heart in the paraconal interventricular groove. Both of these branches send large rami over the surface of the left ventricle. A septal branch courses into the interventricular septum, which it supplies.
The great cardiac vein, which begins in the paraconal interventricular groove, returns blood supplied to the heart by the left coronary artery. The coronary sinus is the dilated terminal end of the great cardiac vein and empties into the right atrium.
Dissect: Identify the origins of the coronary arteries in the ascending aorta by passing a probe through the openings as they branch from the aorta. You need not determine which is right and left.
Identify the great cardiac vein in the coronary groove. Identify the coronary sinus (widening of the great cardiac vein at its terminal end) and the opening of the coronary sinus into the right ventricle.
- Fossa ovalis
Review videos
Understanding how the heart is positioned within the thorax – 1 min
Heart review, Spradley – 23 min
Heart review, Walker – 14 min
Adult vs fetal circulation (lecture type review) – 14 min
Horse pericardium – 30 sec
Terms
Heart and Pericardium |
|
| Features | Species |
| Pericardial (mediastinal parietal) pleura | All |
| Mediastinum | All |
| Pericardium | All |
| Fibrous pericardium | All |
| Parietal pericardium | All |
| Pericardial cavity | All |
| Visceral pericardium (epicardium) | All |
| Phrenicopericardial ligament | Carnivores (in situ only) |
| Sternopericardial ligament | Ungulates (in situ only) |
| Heart | All |
|
Cardiac notch (on lungs) |
All |
|
Coronary groove (sulcus) |
All |
|
Great cardiac vein |
All |
|
Subsinuosal interventricular groove (sulcus) |
All |
| Paraconal interventricular groove (sulcus) | All |
| R/L coronary artery | All (ex situ only-do not need to side) |
| Left atrium | All |
|
Left AV (bicuspid/mitral) valve |
All |
| Left auricle | All |
| Pulmonary vv. | All |
| Right atrium | All |
| Cranial vena cava | All |
| Caudal vena cava | All |
| Coronary sinus and its opening into the right atrium | All |
| Right AV (tricuspid) valve | All |
| Chordae tendineae | All |
| Interatrial septum | All |
| Fossa ovalis/foramen ovale | All (Foramen ovale only in calf) |
| Right auricle | All |
| Right ventricle | All |
| Papillary mm. | All |
| Trabecula septomarginalis | All (know function as well) |
| Pulmonary valve | All |
| Pulmonary trunk | All |
| Pulmonary aa. | All |
| Ligamentum arteriosum | All |
|
Ductus arteriosus |
Calf |
| Patent ductus arteriosus | Conceptual |
| Left ventricle | All |
| Papillary mm. | All |
| Aortic valve | All |
| Chordae tendineae | All |
| Interventricular septum | All |
| Form and Function and Clinical Applications | Notes |
| S1 and S2 heart sounds | When they occur and what causes them |
| Ventricular systole and diastole | Which valves are open/closed during each phase; in what direction is blood flowing |
| SA and AV nodes | Where are they located; what are their functions |
| Pericardial effusion | Define and identify on radiograph and/or echocardiogram |
| Pericardiocentesis | Define; where to perform in all species (ICS and where relative to rib) |
| Points of Maximum Intensity | Know where each valve is most readily auscultated in the domestic species |
| Normal vs. Abnormal Heart Sounds | Know what a normal resting equine, large/small dog, and cat heart sounds like and differentiate it from abnormal |