Lab 5A: Lower Respiratory Tract 1 – Thoracic cavity, pleura, pleural cavities
Learning Objectives
- Recall and compare the musculoskeletal anatomy of the thoracic cavity walls, for the species studied.
- Describe and identify the thoracic inlet and thoracic outlet.
- Describe and identify pleura and pleural cavities.
- Describe and identify the costodiaphragmatic recess and its relationship to the lung.
- Describe and identify the mediastinum and the viscera contained within.
- Identify the two folds of ‘connecting’ pleura
- Associate the normal anatomy with clinical procedures and diseases.
Lab Instructions:
Dissection is performed by students on carnivore cadavers. Become familiar with the anatomy described in the carnivore and then move to the prosected ungulate cadavers to learn comparative and novel features in those animals. Refer to and learn from the wet and dry specimens available in the lab.
Observe: Following the cardiovascular unit, a thoracic limb has been removed and that same side of the thorax is open on the carnivore cadaver, and the lung has been removed. Locate the removed lung, and keep available for studying. During this lab the other thoracic limb will be removed and that side of the thorax will be opened – see instructions below.
Thoracic wall review, all species – musculoskeletal system material (not examined this unit)
We studied the anatomy of the thoracic wall from a musculoskeletal perspective in Semester 1. Given its direct association with the respiratory system this is a good time to remind ourselves of that anatomy. Before we open the thorax, take the time to consider what has been previously learnt. To follow are sections of copied and edited content from the relevant MSK labs. Refer back to the Musculoskeletal System lab book for complete details.
The bony thoracic wall consists of thoracic vertebrae dorsally, ribs on left and right sides, and the sternum ventrally. There is an ‘inlet’ and an ‘outlet’ to the thoracic cavity. There is considerable variation in the number of vertebrae and ribs between the species we are studying, whereas the number of sternebrae are relatively similar, in the 6-8 range.
Thoracic vertebrae – comparative
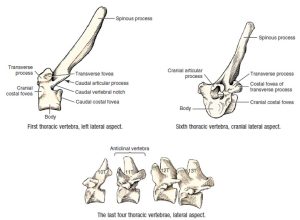
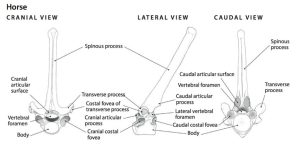
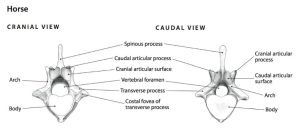
Carnivores have 13 thoracic vertebrae, and ruminants do too. Horses, with their long, barrel-shaped thorax, typically have 18 (17-19 range) thoracic vertebrae, and pigs, 14-15. Thoracic vertebrae have a prominent spinous process, a body, an arch (consists of two pedicles and a lamina), cranial and caudal articular processes, and transverse processes. The thoracic vertebrae are also modified for articulation with the ribs. Sites where ribs join to a vertebra are identified as shallow depressions in the vertebra called costal fovea (costa [L] = rib; fovea [L] = pit, small depression). Recall that the 11th thoracic vertebra is the anticlinal vertebra in the canine.
- Dog thoracic vertebrae. 1
- A cranial thoracic vertebra of the horse; cranial, lateral, and caudal views. 5
- A caudal thoracic vertebra of the horse, cranial and caudal views. 5
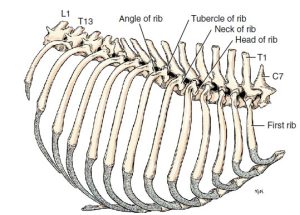
Ribs – comparative
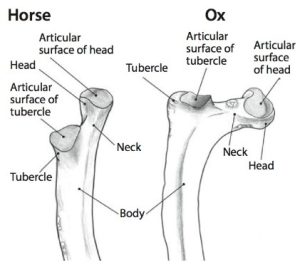
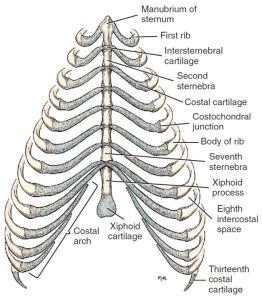
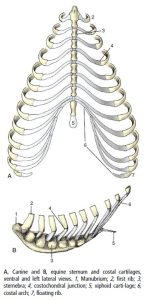
The number of rib pairs matches the number of thoracic vertebrae! The majority of the rib is bone, with features including a head, neck, tubercle, and body. Ventrally, the rib continues as a cartilaginous structure, the costal cartilage. The costochondral junction refers to the junction between osseous and cartilaginous rib. Costal cartilages of sternal ribs articulate directly with the sternum (8-9 pairs). The remaining caudally-located rib pairs (asternal ribs) articulate with each other via their costal cartilages. The continuous line of united costal cartilages forms the costal arch, which also represents the caudal margin of the thorax. The thirteenth pair of ribs in carnivores often end freely in the flank (‘floating’ ribs) rather than being integrated into the costal arch. Horses and ruminants do not usually have floating ribs. The space between adjacent ribs, filled with muscles, neurovascular and other soft tissues, is called the intercostal space (ICS).
- Ribs and sternum of the dog, right lateral aspect. 1
- Proximal portion of a rib of the horse and ox. 5
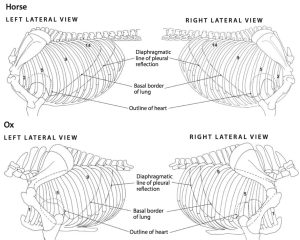
- Left and right lateral views of the thorax, lungs, and extent of pleurae in the horse and the ox. 5
Sternum – comparative
The sternum is composed of a column of bony segments, the sternebrae (singular, sternebra) united by intervening cartilages, or sometimes fused together. Carnivores have eight (8) sternebrae, the horse and ruminant seven (7), and the pig, six (6). The first sternebra, also known as the manubrium, ends cranially in a clublike enlargement. The last sternebra is flattened dorsoventrally and is called the xiphoid process. The caudal end of this process is continued by a thin plate, the xiphoid cartilage.
- Ribs and sternum of the dog, ventral aspect. 1
- Canine and equine sternum and costal cartilages. 8
A few thoracic wall muscles
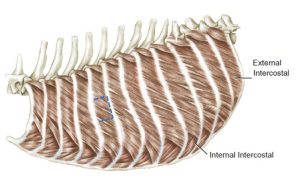
External intercostal mm. have fibers that run caudoventrally in the intercostal space. The external intercostal mm. extend ventrally, only to the level of the costochondral junction. They function in respiration by drawing the ribs together.
The internal intercostal mm., the next muscle layer deep to the external intercostal mm., are easily differentiated from the external intercostal mm. because their fibers run cranioventrally from the cranial border of one rib to the caudal border of the rib cranial to it. The internal intercostal mm. occupy the entire intercostal space, dorsally down to the sternum. These muscles function similar to that of the external intercostal mm., by drawing the ribs together.
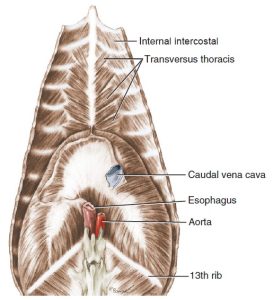
The transversus thoracis m. lines the internal ventral thoracic cavity on the left and right sides, extending from the sternum to the costochondral level. The muscle is visible in an opened thoracic cavity. This muscle assists with expiration. Recall that the internal thoracic a. lies deep to the transversus thoracis m., running parallel to the sternum.
- Deep muscles of thorax of the dog, lateral aspect. 1
- Transversus thoracis muscle of the dog. 1
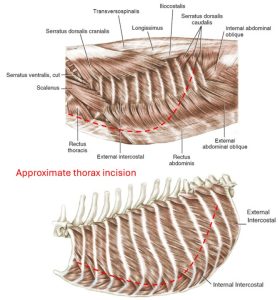
Clinical application – thoracotomy, sternotomy, managing thoracic wall wounds
Intercostal thoracotomy is the most common surgical approach to the thoracic cavity. Incision and retraction of thoracic wall muscles is necessary, starting superficially with the cutaneous trunci and latissimus dorsi mm. Ventrally, the internal thoracic a. should be avoided when an incision is extended in that direction. The main limitation of an intercostal thoracotomy is access to the opposite-side pleural cavity. Primarily used in small animal surgery, median sternotomy is an alternative approach, providing access to the entire thoracic cavity. A good 3D visualization of the thoracic wall anatomy aids in recognizing the location and depth of thoracic wall wounds. A closed pleural cavity that becomes open during wound debridement or through ongoing tissue necrosis would ideally be pre-emptively considered and planned for.
Content examinable from this section onwards
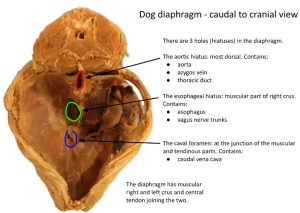
Thoracic cavity boundaries and the inlet and outlet
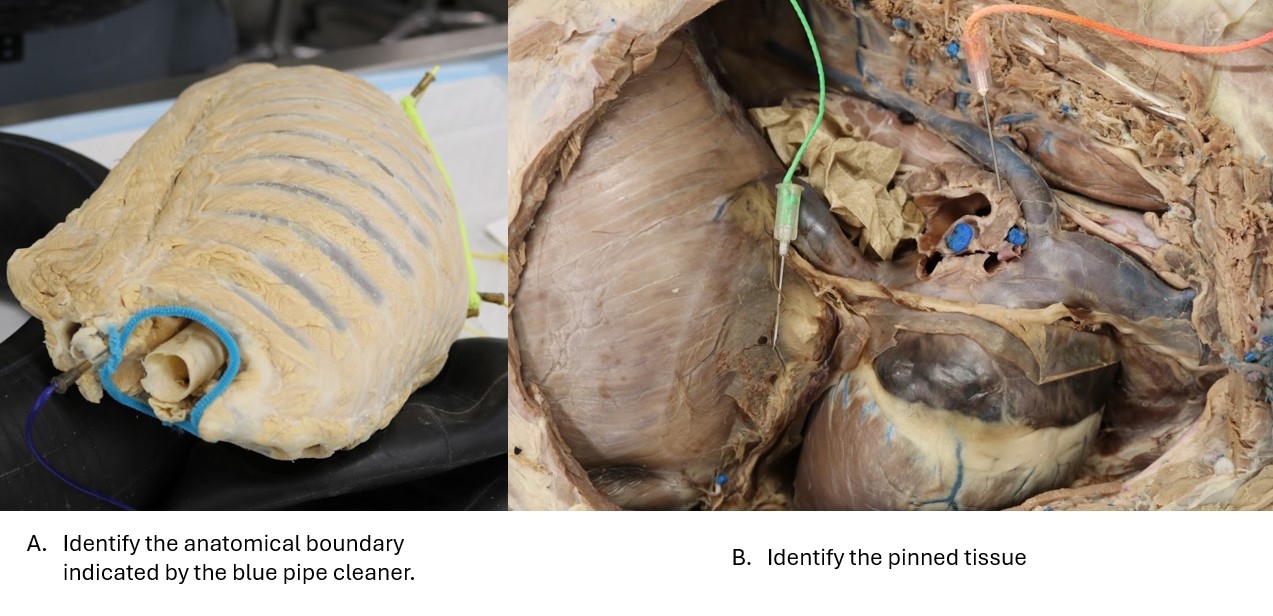
The thoracic cavity is bound by bone, cartilage and muscle. Cranial, caudal, dorsal, ventral and lateral boundaries exist. The cranial boundary is termed the thoracic inlet, defined by the manubrium (first sternebrae), the pair of first ribs and the first thoracic vertebrae (T1). Neck viscera pass through the thoracic inlet to enter the thoracic cavity. The caudal boundary is defined as the thoracic outlet. The thoracic outlet is bound by the last thoracic vertebra dorsally, the last rib pair and the costal arches laterally, the xiphoid process ventrally (i.e. the most caudal sternabra), and the diaphragm. The dorsal boundary of the thoracic cavity is formed primarily by the thoracic vertebrae, along with epaxial and hypaxial muscles associated with this part of the vertebral column. The pairs of ribs and their costal cartilages and intercostal mm. form the lateral boundaries. The sternum and ventral thoracic mm. (rectus thoracis m. and transversus thoracis m.) form the ventral boundary of the thoracic cavity.
Observe: Study the boundaries of the thoracic inlet and outlet on a skeleton. Describe them. Then review the boundaries again from the internal perspective, once both sides of the thorax are open.
Dissect: Alright, time to remove a limb and to open the remaining side of the thoracic cavity, following the same instructions from previous units:
- All skin should have been reflected by now – if not remove any remaining skin over the closed thorax.
- Amputate the thoracic limb that was previously dissected for vessel anatomy – transect the extrinsic muscle attachments and transect the brachial plexus and large vessels in the axilla. Store the limb in the cadaver bag.
- Elevate and excise and discard remaining thoracic wall muscles and stumps of extrinsic muscles to be able to view the external intercostal mm. Do not disturb the external abdominal oblique m.
- Take a moment to count ribs and intercostal spaces….where would you do a thoracocentesis? (scroll down a bit for a few hints)
- Incise through rib cartilage about 2-3 cm lateral to the sternum at ribs 2-8. Incise the muscles between rib cartilages and make an opening into the thoracic cavity.
- Reach inside the thorax and feel the line of pleural reflection by extending fingers caudally. Use care when doing so, as the incised ribs may be sharp. The line of pleural reflection is where the costal pleura sharply turns from lining the ribs to become the diaphragmatic pleura, lining the diaphragm. This is where the diaphragm is attached to the rib cage.
- Cut through the thoracic wall from rib 8 ventrally to the caudodorsal corner, staying about 2 cm cranial to the line of pleural reflection so as to not enter the abdomen.
- Making a full thickness wall incision ventral to dorsal in ICS 1, taking care not to cut deeper cavity tissues.
- An assistant stands on the other side of the cadaver, grasps the cut edge of the thoracic wall and elevates it to create an opening to see inside and to insert bone cutters.
- Reach inside the thoracic cavity with bone cutters, and snip each rib as far dorsally as possible (just before they articulate with the vertebrae).
- As the ribs are snipped, the assistant is able to further open the thoracic cavity (and their arms stop trembling). Return to ribs to complete cuts as needed and cut muscles in between the ribs to help hinge open the thoracic wall segment. It should lie open without a need to hold it when all is adequately transected.
- Lastly, return to rib 1 and now with a clear view of the cranial thoracic cavity it can be removed without disturbing underlying tissues. Leave the lung in place for now.
Helpful videos
- Video: Dr. Gerard reviews structures and the process of opening the canine left thoracic cavity – 22 minutes. Has sound.
- Video: Dr. Gerard quickly opens the canine right thoracic cavity – 5 minutes. Has basic instructions written on screen; no sound needed. Note – while he and other instructors may partially amputate the right limb, students should complete the amputation.
- Video: Lindsey opens the feline right thoracic cavity – 12 minutes. No sound needed.
Let’s move into examining the internal anatomy of the thoracic cavity as it relates primarily to the respiratory system. Portions of this material were introduced in the Cardiovascular system because the anatomy is relevant to both systems.
Pleura and pleural cavities
Observe: With both sides of the thorax now open we can examine and identify many features and structures of the internal thoracic cavity through observation and palpation, without the need to dissect, just yet. Read the following descriptions and be able to identify and describe any bolded terms. Examine both sides of the thorax to gain an understanding of this anatomy with the lungs in situ or removed.
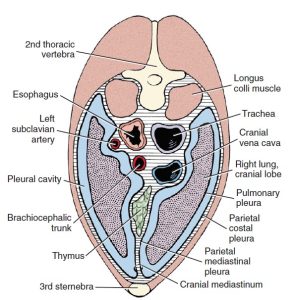
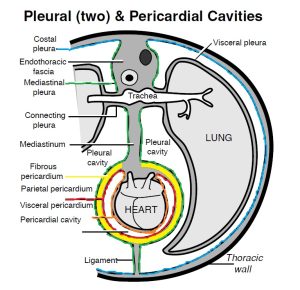
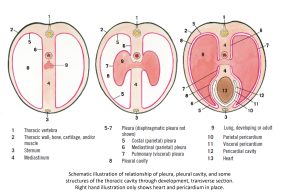
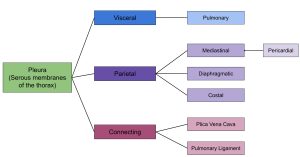
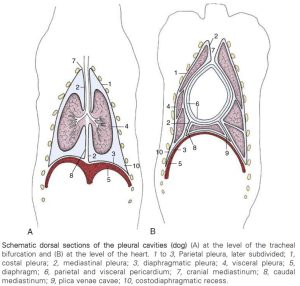
The pleurae (singular pleura) are serous membranes that envelop the lungs and line the internal walls of the thorax. The pleurae form separate right and left closed ‘pleural sacs’, creating the pleural cavities (i.e. there is one thoracic cavity divided into a left and right pleural cavity). These “potential spaces” typically contain only a small amount of serous fluid – just enough to lubricate movement of the lungs. The cupula pleura refers to the cranial blind end of the pleural sac and cavity, at the thoracic inlet. Between the pleural cavities, on midline, is the mediastinum, a structure that will be described in detail shortly and that has been considered already in the cardiovascular unit. Pleura is subclassified as visceral, parietal, or ‘connecting’, depending on its location.
The visceral (or pulmonary) pleura attaches to and lines the entire surface of the lung, completely wrapping it in the membrane, diving into the fissures and back out, following all contours. The pulmonary pleura, at the root of the lung, is continuous with the mediastinal pleura.
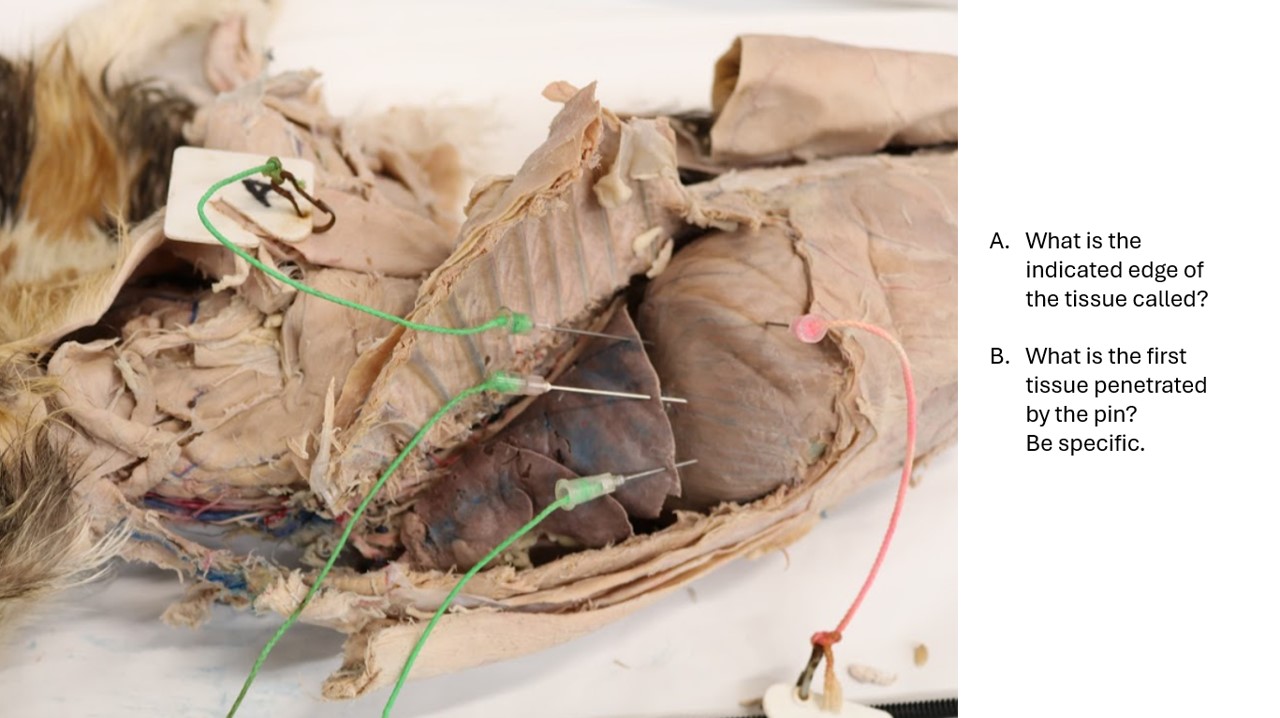
The parietal pleura (parietal means wall) is attached to the thoracic wall by the endothoracic fascia. Endothoracic fascia lines the muscles and bones of the internal lateral thoracic walls. Parietal pleura is divided into costal, diaphragmatic, and mediastinal parts. Each of these is named after the region or surface it covers. Costal pleura covers the inner surfaces of the ribs and their associated intercostal and transversus thoracis muscles, forming a layer over the endothoracic fascia. Diaphragmatic pleura covers the cranial (i.e. thoracic) surface of the diaphragm. The line of pleural reflection (LOPR) is where the costal pleura sharply turns from lining the ribs to become the diaphragmatic pleura, lining the diaphragm. It is a hairpin turn. The line of pleural reflection defines the caudal most extent of the pleural cavity. We move from the thoracic cavity to the abdominal cavity when passing through the diaphragm. Similarly, if we passed an instrument through the LOPF cranial to caudal it would pass from the pleural cavity into the abdominal cavity. Mediastinal pleura covers the walls of the thoracic cavity midline partition, the mediastinum. Mediastinal pleura is continuous with pulmonary pleura at the root of the lung (see Lab 7A). Where the mediastinal pleura is layered over the heart it is referred to as pericardial mediastinal pleura or simply pericardial pleura. The various, named sections of pleura are part of one continuous layer. So one could place a probe on the costal pleura, for example, and move around the entire parietal and visceral pleural surfaces of the pleural cavity, without needing to lift the probe off the pleural surface.
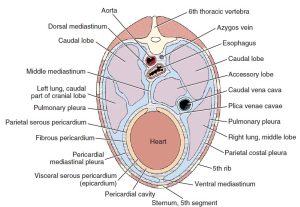
-
Transverse section of thorax through cranial mediastinum
and lungs. 1
- Transverse section of thorax through heart and lungs. 1
- Pleural and pericardial cavities.
- Illustration of relationship of pleura, pleural cavity and some structure of the thoracic cavity through development. 4
- Pleura classification
Observe: Observe the open cavity with the lung still attached.
There is an interplay of anatomical features to consider at this time. As lungs expand and contract with inspiration and expiration, they occupy a constantly altering volume of the thoracic cavity. As the lung expands with inspiration, the caudoventral margin moves caudally into a potential space between the parietal pleura of the ribs and the diaphragm. This space is called the costodiaphragmatic recess (fyi, there are other anatomical recesses in the pleural cavity). The caudal extent of the costodiaphragmatic recess is defined by the previously mentioned line of pleural reflection, i.e.. the most caudal extent of the pleural cavity. The basal border of the lung is that margin of the lung where the costal and diaphragmatic surfaces of the lung meet; it is the caudal-most border of the lung as seen from a lateral view. The border is approximated externally as a caudodorsally sloping line extending from the 6th costochondral junction to the dorsal aspect of the 11th intercostal space. Logically it follows that this lung border moves in relation to the thoracic wall with lung inflation and deflation. By definition, the costodiaphragmatic recess is bound cranially by the basal border of the lung and as already stated, caudally by the line of pleural reflection. Again, it follows that this recess width (as viewed from a lateral perspective) narrows and widens as lungs move in and out of the space with respiration. The lung does not typically occupy the entire recess space, even at full inspiration. When performing a thoracocentesis, the costodiaphragmatic recess ostensibly provides a space to reduce the risk of puncturing lung tissue.
- Schematic dorsal sections of the pleural cavities of the dog. 7
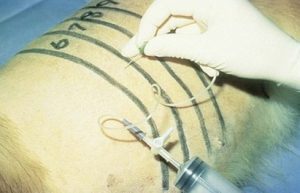
Clinical application: Thoracocentesis (thoracentesis, chest tap)
Thoraco-(from Thorax [Gk] – chest) and centesis (from Kentesis [Gk] – a pricking, puncturing) means to pass a device (e.g. a needle, catheter, chest tube) through the thoracic wall, into the thoracic cavity (specifically, the pleural cavity, and pleurocentesis or pleural tap is occasionally used). It is an important clinical procedure involving the thoracic wall anatomy. The pleural cavity (having now been examined) is a space, that normally is ’empty’ and in disease states it can fill with air or fluid (or a mass). Clinically we need to remove this air or fluid and to access the pleural cavity we may perform a thoracocentesis. Often this is done under emergency conditions to alleviate respiratory distress. We want to be caudal to the heart and still access the more cranioventral pleural cavity for optimal fluid removal. For air removal we may be more caudal and dorsal (particularly in a standing animal, as is common in large animal thoracocentesis). In small animals, low stress restraint, in sternal recumbency or standing, if possible, is also ideal.
The general rule of thumb, across small and large animals, for the anatomical approach for thoracocentesis to drain fluid is:
- 7th-8th ICS; on a level about halfway between elbow and shoulder joints i.e. just above the costochondral junction; on the cranial margin of the rib! (so which rib numbers would we be thinking here?)
Why the cranial margin of the rib? You should be very aware of the reason now. If not, refer back to the cardiovascular unit.
- Horse thoracocentesis ivis.org
- Dog thoracocentesis vettimes.co.uk
- Dog thoracocentesis veteriankey.com
Cat thoracocentesis
Horse chest tube placement
Mediastinum
Observe: Firstly, review the below details and observe the structures and regions of the mediastinum in the pleural cavity that is without a lung.
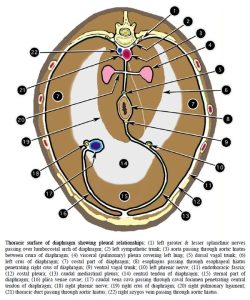
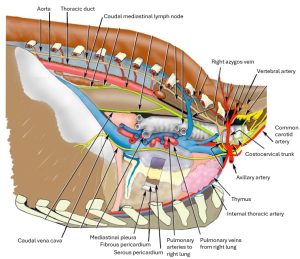
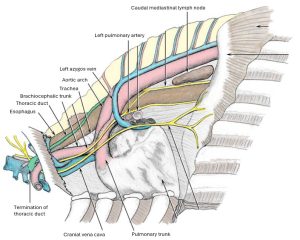
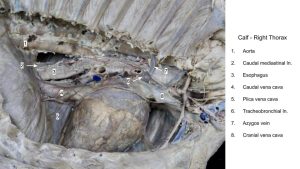
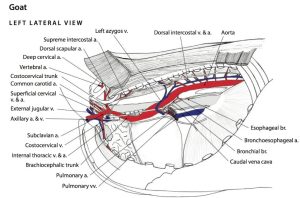
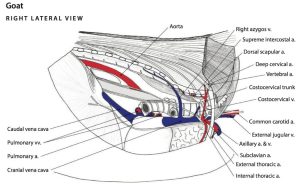
Returning to the mediastinum (literally referring to the ‘middle of the thoracic cavity’), this structure is defined as the left and right mediastinal pleurae and the midline ‘compartment’ between them. Between the pleural walls, i.e. within the ‘compartment’ of the mediastinum, are located all the visceral structures of the thorax, except the lungs. There is no open space in the compartment, it is filled with viscera and connective tissue. The mediastinal viscera includes thymus, lymph nodes and vessels, heart, aorta, trachea (thoracic part), esophagus (thoracic part), vagal nerves, and other nerves and vessels. Previously noted, the pericardial pleura is the specific part of the mediastinal pleura that covers the heart.
The mediastinum can be divided into regions, that are continuous with their adjacent region(s): cranial mediastinum, that lying cranial to the heart; middle mediastinum, that containing the heart; dorsal mediastinum, that dorsal to the heart; ventral mediastinum, that ventral to the heart; and caudal mediastinum, that lying caudal to the heart. The caudal mediastinum is thin ventrally, because this is where the mediastinal pleurae meet each other on midline with very little connective tissue and no viscera intervening. The caudal mediastinum attaches to the diaphragm to the left of the median plane.
- Thoracic surface of diaphragm showing pleural relationships. 2
-
Transverse section of thorax through cranial mediastinum
and lungs. 1
- Transverse section of thorax through heart and lungs. 1
Observe: FYI for now: Note the passage of the esophagus through the cranial, middle, and caudal mediastinum and the esophageal hiatus of the diaphragm. At the esophageal hiatus, a thin layer of pleura, peritoneum, and enclosed connective tissue attaches the esophagus to the muscle of the diaphragm.
Also recall and identify the thymus, tracheobronchial lymph nodes, and the thoracic duct, structures examined in the cardiovascular unit.
- Dog esophageal hiatus in diaphragm.
Two folds of pleura
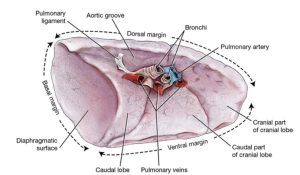
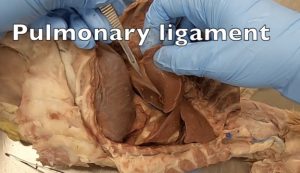
Two folds of pleura, that may be classified as connecting pleura (because they seem like they are), remain to be described and identified. The plica venae cavae is a loose fold (plica = fold) of pleura that surrounds the caudal vena cava (and the right phrenic nerve) and is continuous ventrally with the right caudal mediastinal pleura. The plica vena cava extends from the heart to the diaphragm. The root of the lung (see Lab 7A) is composed of pleura and the bronchi, vessels, and nerves entering the lung. Caudal to the root of the lung the mediastinal and pulmonary pleura remain connected to each other by a ‘bridge’ of pleura, which ends as a free border. This pleural fold is the pulmonary ligament and it anchors the caudal lung lobe to the mediastinum. The pulmonary ligament is present in left and right pleural cavities.
Observe: Identify the plica vena cava in the right pleural cavity. Identify the pulmonary ligament by gently grasping the caudal border of the in situ caudal lung lobe, and retracting it laterally and cranially. The fold of tissue stretched by this retraction and keeping the caudal lung lobe from being further displaced is the pulmonary ligament.
- Left lung of the dog, medial view. 1
- Dog plica vena cava
- Cat pulmonary ligament
Clinical application: lobectomy or pulmonectomy
During thoracic surgery, when indicated, the pulmonary ligament is cut to reflect the caudal lung lobe cranially. This may be part of a lobectomy (lung lobe removal) or pulmonectomy (remove entire lung on one side) procedure.
You know what! We were about to recommend removing the remaining in situ lung at this time, but lets leave it attached, and it will be a good reminder of the pulmonary ligament when the lung is potentially removed.
Comparative Ungulate Anatomy
Observe: Firstly, swipe back to the top of this lab and consider the musculoskeletal anatomy of the thorax, and the thoracic inlet and outlet anatomy. Utilize articulated skeletons and the prosected cadavers.
Observe: Study the ungulate cadavers and specimens to identify the pleurae and features as considered in the carnivore. Lungs have been detached from both sides in the ungulates and will be retrieved and studied in Lab 7A.
Pleura, pleural cavities
As a reminder, the pleura is the serous membrane that lines the walls of the thoracic cavity, envelops the lungs, and forms two closed sacs, creating the pleural cavities. These “potential spaces” typically contain only a small amount of serous fluid – just enough to lubricate movement of the lungs. The cupula pleura is evident on the right side, this being the extension of the pleural cavity cranial to the first rib. The left pleural cavity typically does not exhibit a cupula pleura, in the ungulate.
In the horse, tiny openings develop postnatally between the left and right pleural cavities, in the caudal mediastinum where the two mediastinal pleural walls are adherent to each other. Therefore, the adult horse is considered to have a fenestrated mediastinum. In general, the mediastinum of the horse is much thinner and more delicate than that of the ox, goat, and pig. Thus, the likelihood of air or inflammatory fluid breaking through from one pleural cavity to the other is greater in the horse – that is, a unilateral pneumothorax could become bilateral, and subsequently fatal. Clinically, however, the tiny mediastinal holes may quickly seal (e.g. in pleuritis, i.e. inflammation of the pleura, they may become plugged with fibrin) and the pleural cavities are then considered separate spaces for diagnostics and treatments.
- Thoracic surface of diaphragm showing pleural relationships. 2
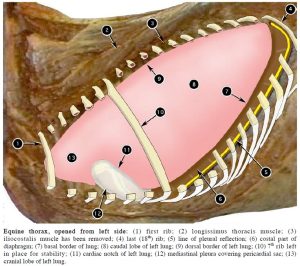
- Equine thorax, opened from left side. 2
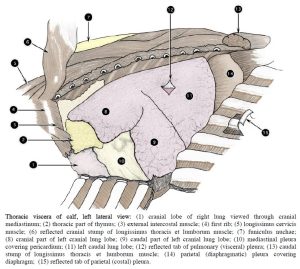
- Thoracic viscera of calf, left lateral view. 2
Clinical application: pleural cavity disease
Pleuritis is inflammation of the pleura, whereas pleuropneumonia affects the pleural cavities and lungs and is far more common in horses than pleuritis alone. A classic history for a horse with clinical signs of pleuropneumonia is having been recently transported for an extended distance/time. Why might this be the case?
Clinical application: cupula pleura vulnerability
Keep the cupula pleura in mind when doing surgery in the caudal part of the neck on the right side, or when dealing with trauma in this area, as it is more possible to penetrate the pleural cavity in this location.
Line of Pleural Reflection
The line of pleural reflection (LOPR) is where the costal parietal pleura and diaphragmatic parietal pleura meet, forming a sharp hairpin turn from one to the other at the caudolateral extent of the pleural cavity. In the horse the line of pleural reflection closely parallels the costal arch, thus following a long, sweeping curve from the 8th costochondral junction to the middle of the last rib (#18). The line of pleural reflection in the ruminant ascends rather abruptly from the 8th costochondral junction, in a slight curve, to the dorsal aspect of the last rib (#13).
- Equine thorax, opened from left side. 2
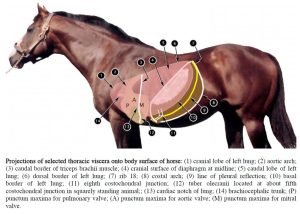
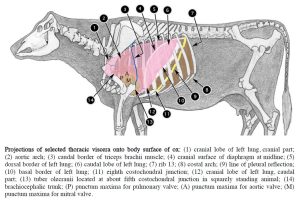
- Projections of selected thoracic viscera onto body surface of horse. 2
- Projections of selected thoracic viscera onto body surface of ox. 2
Observe: On a cadaver or articulated skeleton, trace the approximate line of pleural reflection on the external surface of the thoracic wall, using the landmarks described, in the horse and the ruminant. Then view the LOPR as identified internally at the caudal extent of the pleural cavity. Recognize that the LOPR lies caudal to the basal border of the lung and between the lung and the LOPR is the costodiaphragmatic recess.
Clinical relevance: LOPR and body wall penetrating trauma.
Mediastinum
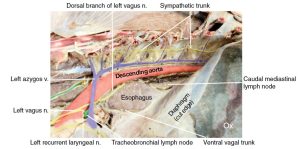
Observe: Identify the mediastinum and its features and regions. Identify the plica vena cava on the right side, related to the caudal vena cava. The cut edge of the pulmonary ligament may be visible, on the caudal lung lobe, and/or on the caudal mediastinum. Note the relative fragility of the mediastinal pleura of the horse compared to the ruminant and pig. Identify the trachea in the mediastinum.
Observe: FYI only – recall and identify mediastinal structures that were studied in the cardiovascular system: thymus (as present), thoracic duct, tracheobronchial lnn., caudal mediastinal ln., great vessels entering and leaving the heart.
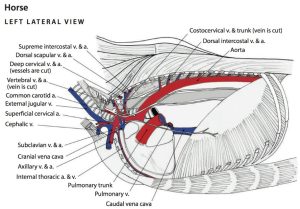
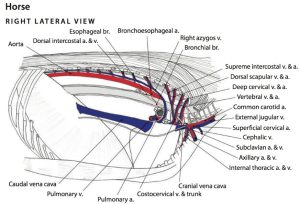
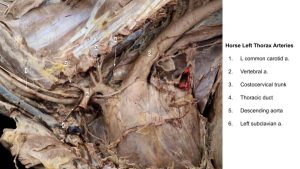
Horse
- Vessels of the thoracic cavity of the horse, left side. 6
- Vessels of the thoracic cavity of the horse, right side. 6
- Horse mediastinum
- Horse mediastinum
Ox
- Thoracic surface of diaphragm showing pleural relationships. 2
- Bovine left caudal thorax.12
-
Bovine left thoracic and cranial abdominal cavities. Identify the major vessels and nerves on the
left thoracic cavity. 12
- Major arteries of bovine mediastinum, right lateral view. 2
- Major structures of bovine mediastinum, left lateral view. 2
- Calf mediastinum
Goat
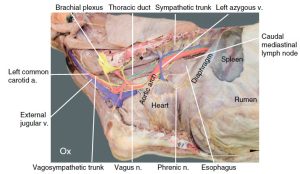
- Vessels of the thoracic cavity of the goat, left side. 6
- Vessels of the thoracic cavity of the goat, right side.6
Review videos
Pleura – Watch until 2 min
Basal border of lung & costodiaphragmatic recess – 2 min, watch until 6:30
Pericardium – Walker, 2 min, watch until 26:00
Pericardium – Spradley, watch until 2 min
Ungulate thorax osteology – Review. 5 min
Horse LOPR – 2 min
Ruminant LOPR – 4 min, watch until 8:00
Plica vena cava – 2 min, watch until 17:30
Pleura and mediastinum – 6 min, watch until 2 min
Terms
| Carnivore and Ungulate | |
| Feature | Species/Comments |
| Thoracic inlet | identify, know boundaries |
| Thoracic outlet | identify, know boundaries |
| Pleura | |
| Visceral (pulmonary) pleura | that covering the lungs |
| Parietal pleura | 3 regions as listed next. |
| Costal pleura | |
| Mediastinal pleura | |
| Pericardial pleura | = the mediastinal pleura covering the heart |
| Diaphragmatic pleura | |
| Pleural cavity | |
| Cupula pleura | all, evident on right side in ungulates. |
| Costodiaphragmatic recess | |
| Line of pleural reflection | |
| Basal border of lung | |
| Mediastinum | divided into 5 regions as listed next: |
| cranial mediastinum | in front of heart |
| middle mediastinum | contains heart |
| dorsal mediastinum | above heart |
| ventral mediastinum | below heart – very narrow region |
| caudal mediastinum | caudal to heart |
| Trachea | thoracic part |
| Plica vena cava | identified on right, related to caudal vena cava |
| Pulmonary ligament | |