Lab 7A: Vessels of the Abdominal Cavity
Learning Objectives
- Identify the arteries that supply the abdominal body wall, and associate each with the corresponding quadrant of the body wall to which it supplies blood.
- Identify the arteries of the abdominal gastrointestinal tract.
- Relate the arteries with the section of bowel that they vascularize.
- Identify the paired arteries of the aorta and what they vascularize.
Lab Instructions
Throughout this lab, in order to identify and follow arteries, it will be necessary to flip from right to and left and back again in your cadaver. Be gentle as you do so in order to not disrupt the abdominal viscera so much that you tear the viscera. Also, this lab assumes your knowledge of the different parts of the gastrointestinal tract, as knowing what section you’re looking at will be the easiest way to associate the artery that is running to that location! Furthermore, dissecting arteries in the abdomen typically requires some disruption of the surrounding mesentery to visualize the vessel. Take care while doing so to avoid unnecessarily transecting an artery that we’re trying to identify.
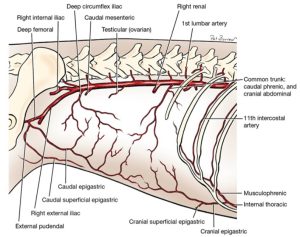
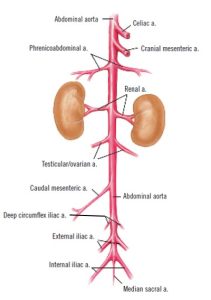
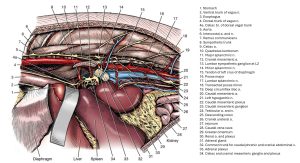
Arterial Supply to the Abdominal Body Wall
When considering the blood supply to the abdominal body wall, we must first begin by subdividing the abdominal body wall into four quadrants on each side; craniodorsal, cranioventral, caudodorsal, and caudoventral (essentially, draw a transverse plane through the umbilicus, and a dorsal plane through the middle of the lateral body wall). The abdominal wall receives its vascular supply primarily through four vessels that are each associated with one of the different quadrants listed above. In brief, these vessels are as follows: the cranial abdominal artery (craniodorsal), cranial epigastric artery (cranioventral), deep circumflex iliac artery (caudodorsal), and caudal epigastric artery (caudoventral). We’ll identify each of these in turn.
Cranial abdominal artery
Dissect: If any remains, reflect the superficial fascia from the lateral abdominal wall.
Emerging from the dorsolateral abdominal wall, caudal to the last rib, are superficial branches of the cranial abdominal artery. The latter arises from a common origin with the caudal phrenic artery off the aorta and perforates the abdominal musculature, which it supplies, to reach the skin, ie it supplies the craniodorsal abdominal wall.
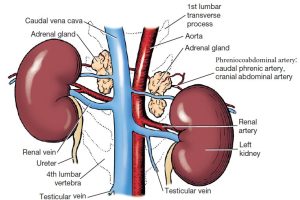
- Kidneys and adrenal glands, ventral view. 1
Observe: Look for arterial branches in the craniodorsal corner of the abdominal wall, right behind the last rib. These branches belong to the cranial abdominal a. We’ll come back to the larger artery from which the cranial abdominal is originating later in this lab.
Cranial epigastric artery
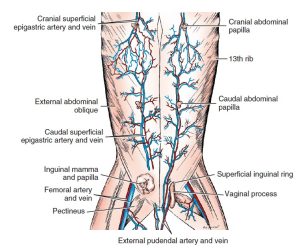
The cranioventral abdominal wall is supplied by the cranial epigastric a. This vessel represents a continuation of the internal thoracic a. (which we identified in the cardiovascular unit, within the thorax). The cranial epigastric a. branches to provide the cranial superficial epigastric artery. This more superficially located vessel supplies the subcutaneous tissues of the ventral abdomen including the mammae. In the female, the cranial superficial epigastric vessels are seen subcutaneously near the cranial abdominal papilla.
- Ventral view of the abdomen of the dog. 1
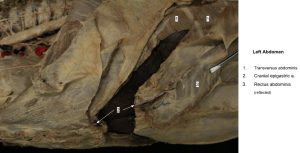
- Cranial epigastric artery (transected)
Observe: Follow the internal thoracic artery from the thoracic cavity caudally into the abdomen, where it changes name to the cranial epigastric artery and is found coursing caudally on the internal surface of the rectus abdominis m. Find the cranial superficial epigastric artery, which branches from it at approximately the level of the costal arch and is found coursing caudally on the external surface of the rectus abdominis m. The branches of the cranial superficial epigastric artery may also be located by blunt dissection: separate the right row of mammae (if observed) from the fascia and turn them laterally to see the branches of the cranial superficial epigastric a.
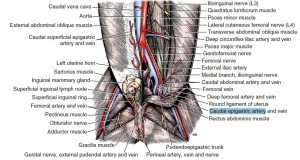
Deep circumflex iliac artery
Cranial to the cranioventral iliac spine, the lateral cutaneous femoral nerve (L4) and the deep circumflex iliac artery and vein perforate the internal abdominal oblique m. and appear superficially. The artery arises directly from the aorta and supplies the caudodorsal abdominal wall.
- Abdominal aorta in relation to epigastric arteries, lateral view.1
- Paired lateral and unpaired ventral branches of the abdominal aorta of the cat, ventral view. 4
- Deep circumflex iliac a.
Dissect: Dissect the cut stumps of these vessels where they perforate the abdominal wall muscles just cranial to the cranioventral iliac spine. You might recall doing this in earlier units!
Caudal epigastric artery
The caudoventral abdominal wall is supplied by the caudal epigastric a. The caudal epigastric a. is readily identified coursing on the deep (internal) surface of the rectus abdominis m. once the abdominal cavity is opened. The subcutaneous tissues of the caudoventral abdomen are supplied by the caudal superficial epigastric artery. The caudal superficial epigastric a. runs cranially to the deep surface of the inguinal mamma and supplies the mammary branches. The artery continues to supply the caudal abdominal mamma and anastomose with branches of the cranial superficial epigastric a. In the male the caudal superficial epigastric a. supplies the prepuce.
- Caudal epigastric artery of the dog. 1
Observe: Identify the caudal epigastric artery on the internal surface of the caudal aspect of the rectus abdominis m.
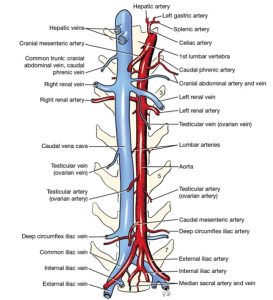
Lumbar Arteries
The paired lumbar arteries leave the dorsal surface of the aorta. Each extends dorsally and terminates in a spinal and a dorsal branch. The spinal branches pass through the intervertebral foramina into the vertebral canal, where they penetrate the dura and arachnoid that surround the spinal cord. Here they anastomose with the ventral spinal artery that is within the subarachnoid space and supply part of the spinal cord. The dorsal branches supply the muscles and skin above the lumbar vertebrae.
- Abdominal aorta in relation to epigastric arteries, lateral view.1
- Branches of abdominal aorta and tributaries of the caudal vena cava, ventral view. 1
- Paired lateral and unpaired ventral branches of the abdominal aorta of the cat, ventral view. 4
Observe: Identify some of the lumbar arteries as they branch off the abdominal aorta and track dorsally.
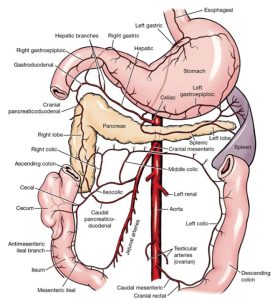
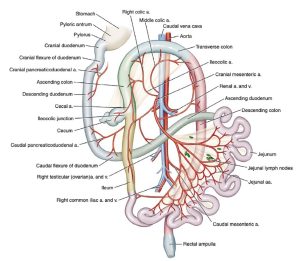
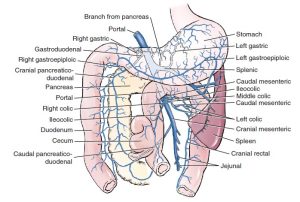
The Celiac Artery and Associated Branches
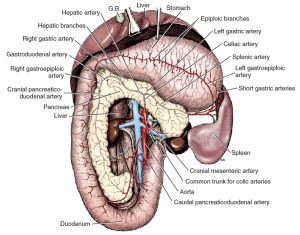
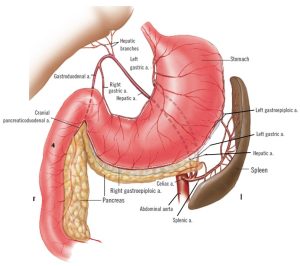
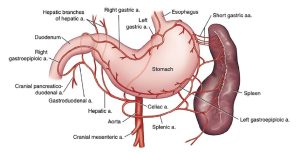
The celiac artery is the most cranial of the three unpaired branches of the abdominal aorta. It is short and arises from the aorta between the crura of the diaphragm. Generally, the celiac artery provides blood to the foregut. It has three branches: the hepatic artery, the left gastric artery, and the splenic artery. The celiac plexus of nerves covers the artery in its course through the mesentery. The hepatic artery is the first branch to leave the celiac artery.
- Branches of celiac and cranial mesenteric arteries with principal anastomoses. 1
- Celiac and cranial mesenteric arteries, ventral aspect. (Stomach reflected cranially.) 1
- Branches of the celiac artery to abdominal viscera of the cat, ventral view. 4
Dissect: Locate and dissect out the celiac artery. Follow it to the origin of the hepatic artery. Then follow the hepatic artery and its branches dorsal to the pylorus between the lesser curvature of the stomach and the liver. Identify these branches as described below.
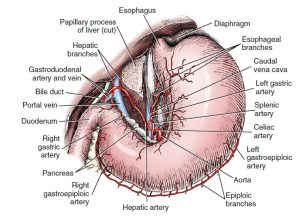
The hepatic artery courses cranially in the cranial border of the mesoduodenum, which is the caudal boundary of the epiploic foramen. It passes to the liver in the hepatoduodenal ligament.
One to five hepatic branches leave the hepatic artery and enter the liver. The cystic artery leaves the last hepatic branch and supplies the gallbladder. It need not be dissected. After giving off branches to the liver, the hepatic artery terminates as the right gastric and the gastroduodenal arteries. This occurs in the lesser omentum.
The right gastric artery is a small artery that extends from the pylorus toward the cardia to supply the lesser curvature of the stomach. It anastomoses with the left gastric artery on the lesser curvature of the stomach.
After splitting away from the right gastric a., the gastroduodenal artery supplies the pylorus and terminates as the right gastroepiploic and cranial pancreaticoduodenal arteries. This occurs at the junction of the greater omentum and the mesoduodenum.
The right gastroepiploic artery enters and runs in the greater omentum along the greater curvature of the stomach. It supplies the stomach and the greater omentum. The right gastroepiploic artery anastomoses with the left gastroepiploic, a branch of the splenic artery.
The cranial pancreaticoduodenal artery follows the mesenteric border of the descending duodenum, where it supplies the duodenum and adjacent right lobe of the pancreas. It anastomoses with the caudal pancreaticoduodenal artery, which is a branch of the cranial mesenteric artery.
- Celiac artery, ventral aspect. (Stomach displaced to left.) 1
- Blood supply of the stomach and the spleen. 9
- Branches of the celiac artery to abdominal viscera of the cat, ventral view. 4
Dissect: Find the right gastroepiploic artery as it courses along the right side of the greater curvature of the stomach. You will likely need to use a probe to gently separate the greater omentum away from the greater curvature of the stomach to better visualize this artery. Next, find the cranial pancreaticoduodenal artery between the right lobe of the pancreas and the descending duodenum. Once again, you will need a probe to gently separate the pancreas away from the duodenum to visualize this artery.
The left gastric artery branches from the celiac and runs in the greater omentum to the lesser curvature of the stomach near the cardia and supplies both surfaces of the stomach. One or more esophageal rami pass cranially on the esophagus. It extends toward the pylorus, where it anastomoses with the right gastric artery.
Dissect: Find the origin of the left gastric artery as it branches from the celiac a. and follow it along the lesser curvature of the stomach, near the cardia of the stomach.
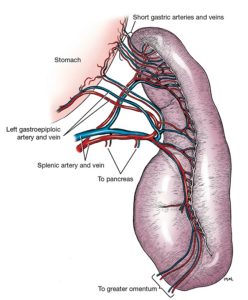
The splenic artery crosses the dorsal surface of the left lobe of the pancreas in the deep leaf of the greater omentum—to which it may supply branches—before dividing into dorsal and ventral splenic branches that enter the hilus of the spleen on its visceral surface. The dorsal branch gives rise to several arteries that enter the dorsal end of the spleen and a few short gastric arteries that course in the gastrosplenic ligament to the greater curvature of the stomach on the left side. The dorsal splenic branch continues as the left gastroepiploic artery on the greater curvature of the stomach. At the pyloric end of the stomach, the left gastroepiploic artery anastomoses with the right gastroepiploic artery, a branch of the hepatic artery. The ventral splenic branch supplies the rest of the spleen by numerous branches that enter at the hilus. Variations in this pattern exist, and you may find that the ventral branch of the splenic, rather than the dorsal branch, gives rise to the left gastroepiploic artery.
- Blood supply of the spleen. 1
Dissect: Find the origin of the splenic artery as it branches from the celiac artery and follow it and its branches as described above.
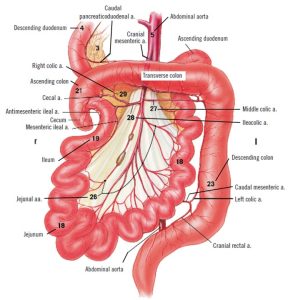
The Cranial Mesenteric Artery and Associated Branches
The cranial mesenteric artery leaves the aorta just caudal to the celiac artery. It is surrounded proximally by the cranial mesenteric plexus of nerves and partly by the cranial mesenteric ganglion. Peripheral to the ganglion are the mesenteric lymph nodes and branches of the portal vein. Generally, the cranial mesenteric artery provides blood to the midgut.
Dissect: Locate the cranial mesenteric artery as it branches from the abdominal aorta. It should be just caudal to the celiac artery, and you will likely need to separate some peritoneum and nervous tissue that wraps around the artery to better visualize it. Follow its branches to the organ(s) which they supply, as described below.
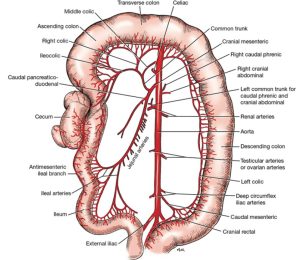
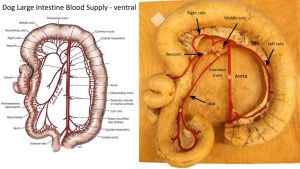
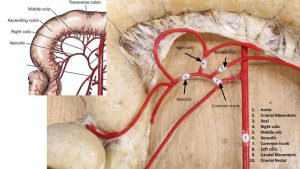
The middle colic, right colic, and ileocolic arteries arise from a common trunk from the cranial mesenteric artery and course through the mesocolon.
- Branches of cranial and caudal mesenteric arteries, ventral aspect. 1
- Dog colon blood supply
- Dog colon blood supply
- Branches of cranial mesenteric and caudal mesenteric arteries to abdominal viscera of the cat, ventral view. 4
Dissect: Reflect the small intestine caudally and expose the colon cranial to the root of the mesentery. Dissect the blood supply to the colon and cecum (i.e., the common trunk from which the middle colic, right colic, and ileocolic aa. arise) within the mesocolon. Identify all of the following branches that are in bold below.
The middle colic artery, the first branch from the common trunk, runs cranially in the mesocolon to the mesenteric border of the left colic flexure and descending part of the colon. It bifurcates near the left colic flexure. One branch runs distally in the descending mesocolon, supplies the descending colon, and then anastomoses with the left colic artery, a branch of the caudal mesenteric artery. The other branch passes to the right and forms an arcade with the smaller right colic artery and supplies the transverse colon.
The right colic artery runs in the right mesocolon toward the right colic flexure, giving off branches to the distal part of the ascending colon and the adjacent transverse colon. It forms arcades with the middle colic artery and the colic branch of the ileocolic artery.
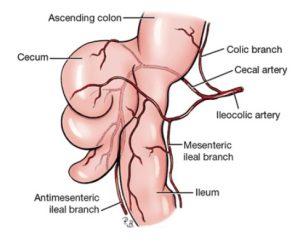
The ileocolic artery supplies the ileum, cecum, and ascending colon. It is closely associated with the right colic lymph node. Its 3 branches are:
- The colic branch of the ileocolic a. supplies the first part of the ascending colon.
- The cecal a. crosses the dorsal surface of the ileocolic junction and supplies the cecum and continues as the antimesenteric ileal a. to supply that side of the ileum.
- Mesenteric ileal a. continues the ileocolic artery in the mesentery attaching to the ileum and anastomoses with ileal arteries of the cranial mesenteric artery.
- Terminations of ileocolic artery. 1
- Branches of cranial and caudal mesenteric arteries, ventral aspect. 1
The caudal pancreaticoduodenal artery arises from the cranial mesenteric artery close to the common trunk for the colon. It runs to the right in the mesoduodenum to the descending portion of the duodenum near the caudal flexure. It supplies the descending duodenum and the right lobe of the pancreas and anastomoses with the cranial pancreaticoduodenal artery. The caudal pancreaticoduodenal artery also branches to supply the caudal flexure and ascending duodenum.
- Branches of celiac and cranial mesenteric arteries with principal anastomoses. 1
- Dog intestinal tract. 9
Dissect: Find the caudal pancreaticoduodenal artery as it branches from the cranial mesenteric artery. Follow it to the aboral portion of the descending duodenum. It runs cranially in between the pancreas and descending duodenum until it forms an anastomosis with the cranial pancreaticoduodenal artery, which you’ll recall is a branch of the gastroduodenal artery (which is a branch of the hepatic artery, which is a branch of the celiac artery).
The jejunal arteries arise from the caudal side of the cranial mesenteric artery. They form arcades in the mesentery close to the jejunum.
Observe: Observe these jejunal arteries in the mesojejunum. When performing a resection and anastomosis of the jejunum (usually to remove a foreign body or mass), it is important to properly ligate these vessels and to transect the length of bowel appropriately to ensure the bowel which remains is still well vascularized.
The ileal arteries are the terminal branches of the cranial mesenteric artery and these will anastomose with the mesenteric ileal branch of the ileocolic artery.
Observe: Observe these ileal arteries within the mesentery of the ileum.
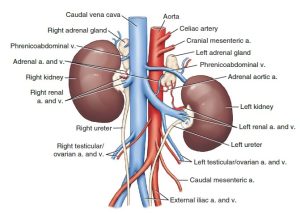
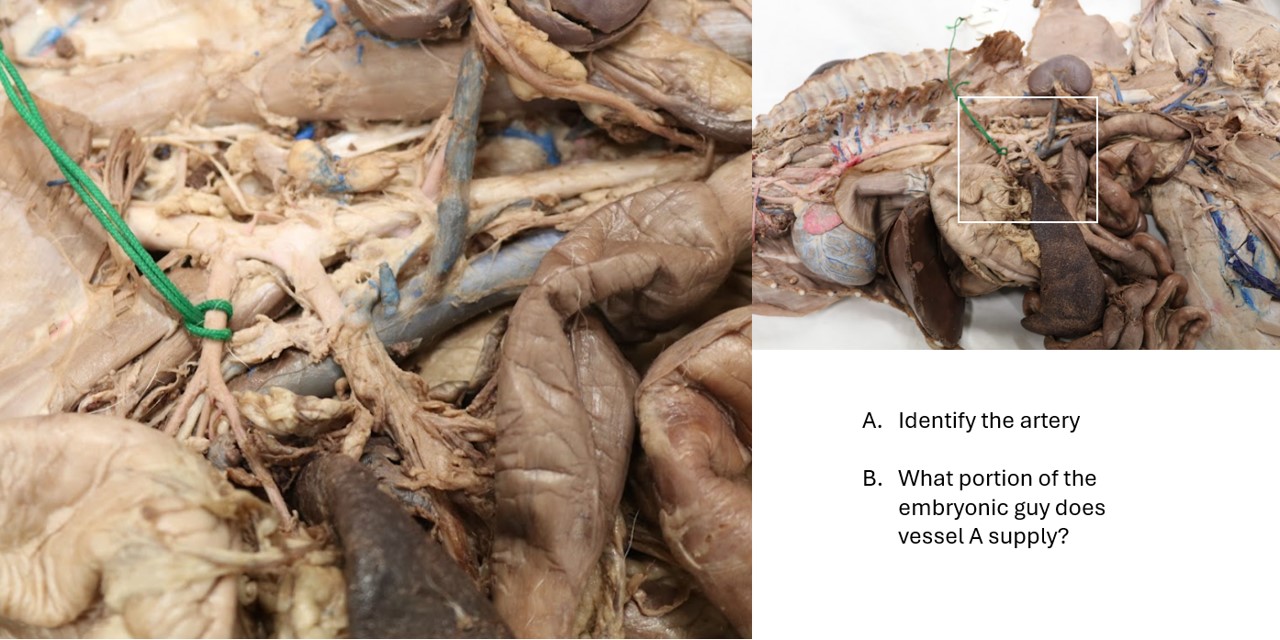
Phrenicoabdominal Arteries
The paired phrenicoabdominal aa. arise from the aorta between the cranial mesenteric a. and renal arteries. The phrenicoabdominal artery is the common trunk of the caudal phrenic and cranial abdominal arteries. It crosses the ventral surface of the psoas muscles dorsal to the adrenal gland. The caudal phrenic artery runs cranially to supply the diaphragm. The cranial abdominal artery continues into the craniodorsal abdominal wall and ramifies between the transversus abdominis and the internal abdominal oblique, where it was previously dissected.
- Kidneys and adrenal glands, ventral view. 1
- The relationship of the adrenal glands to the regional anatomy. 9
Dissect: Find the left phrenicoabdominal artery and vein as they cross over the left adrenal gland, just cranial to the kidney. Dissect it as it branches into the cranial abdominal and phrenic arteries. Students are responsible for identifying the left cranial abdominal artery but not the phrenic. Note that the cranial abdominal arteries supply the muscles of the right and left cranial quadrants of the abdominal wall.
The adrenal gland may receive branches from the aorta or caudal phrenic, renal, or lumbar arteries. The adrenal glands are light-colored and are located at the cranial aspect of each kidney. Each gland is crossed ventrally by the phrenicoabdominal vein, which leaves a deep groove on its ventral surface.
Observe: Identify the left and right adrenal glands in your cadaver, note the presence of the phrenicoabdominal vein crossing over the ventral surface of the gland.
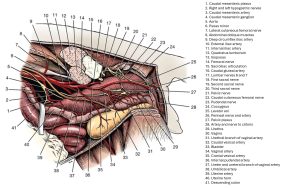
Renal and Gonadal Arteries
The renal arteries leave the aorta at different levels. The right one arises cranial to the left, in conformity with the more cranial position of the right kidney. The right renal a. is longer than the left and lies dorsal to the caudal vena cava.
The ovarian artery of the female is homologous to the testicular artery of the male (we can refer to them as the “gonadal arteries” if we aren’t specifying the sex of the animal). This paired vessel arises from the aorta about halfway between the renal and external iliac arteries. The ovarian artery varies in size, position, and tortuosity, depending on the degree of development of the uterus. Each ovarian artery divides into two or more branches in the mesovarium just medial to the ovaries. Branches supply the ovary and its bursa and the uterine tube and horn. The branch to the uterine horn anastomoses with the uterine artery, a branch of the vaginal artery that runs cranially in the mesometrium. The testicular artery leaves the aorta in the midlumbar region and crosses the ventral surface of the ureter. The testicular artery, vein, and nerve plexus lie in a peritoneal fold, the mesorchium, which can be followed to the level of the vaginal ring. The right testicular and ovarian veins enter the caudal vena cava near the origin of the artery from the aorta. However, the left testicular and ovarian veins usually enter the left renal vein. This is important surgically. The ovarian and testicular arteries will be reviewed in the urogenital unit.
- Exposure of abdominal autonomic nervous system on left side. 1
- Kidneys and adrenal glands, ventral view. 1
Observe: Locate and identify the renal and testicular/ovarian arteries as they branch from the abdominal aorta.
Caudal Mesenteric Artery
The caudal mesenteric artery is unpaired and arises near the termination of the aorta. It enters the descending mesocolon and runs caudoventrally to the mesenteric border of the descending colon, where it terminates in two branches of similar size. The left colic artery follows the mesenteric border of the descending colon cranially to anastomose with the middle colic artery. The cranial rectal artery descends along the rectum and anastomoses with the middle rectal artery from the prostatic or vaginal artery.
- Autonomic nerves and vessels of pelvic region, left lateral view. 1
- Branches of cranial mesenteric and caudal mesenteric arteries to abdominal viscera of the cat, ventral view. 4
Dissect: Locate the caudal mesenteric artery as it branches from the caudal abdominal aorta. It was previously dissected in order to observe the caudal mesenteric ganglia and plexus (remember??). Continue to trace it as it branches into the left colic and cranial rectal arteries, which supply the second half of the descending colon and cranial rectum, respectively.
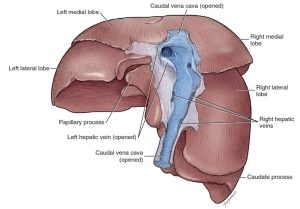
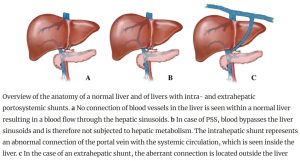
Hepatic Portal Venous System
A venous portal system consists of a capillary bed interposed between veins returning blood to the heart. The hepatic portal vein carries venous blood to the liver from abdominal viscera such as the stomach, the small intestine, the cecum, the colon, the pancreas, and the spleen. As the portal vein enters the liver in the hepatoduodenal ligament, it divides into a short right and a long left branch. The right branch supplies the right lateral lobe and caudate process of the caudate lobe. The left branch supplies the other lobes. Within these lobes the portal venous branches give rise to a large array of hepatic sinusoids that form an extensive capillary bed. These sinusoids are drained by larger branches that give rise to a variable number of hepatic veins. The hepatic vv. drain into the caudal vena cava as it traverses the dorsal aspect of the liver, on its way to the right atrium of the heart.
Observe: Retract the caudate process of the caudate lobe of the liver from the cranial duodenal flexure. Find the portal vein in the hepatoduodenal ligament at the ventral border of the epiploic foramen.
Blood from the gastrointestinal system (stomach, intestines, pancreas, and spleen) must pass through the liver so that toxins from food digestion can be removed. This occurs through the hepatic portal vein. Once it has passed through the liver, it flows to the caudal vena cava via the hepatic veins. This blood is referred to as the functional blood of the liver. Recall that nutrient supply to the liver is via the hepatic arteries (branches of the heptic artery/branch of cranial mesenteric a.). This blood also exits the liver via the hepatic veins.
- The portal vein, ventral aspect. 1
- Dorsal view of the liver to show hepatic veins. 1
Clinical Application
Portosystemic Shunt
Some animals suffer from a portosystemic shunt. External portosystemic shunts are vascular anomalies located outside of the hepatic parenchyma. They are extra vessels running from the portal vein to the caudal vena cava or other vein. They may be congenital (from birth) or acquired. In these cases, venous blood returning to the heart from the digestive system does NOT pass through the liver parenchyma. Internal portosytemic shunts (most often congenital), or portal vein hypoplasia, occurs when microscopic shunting of the blood in the liver occurs due to small or absent intrahepatic portal vessels. In either external or internal shunting, blood is not rid of toxins, especially ammonia, which will accumulate over time and can cause seizures in affected animals. In the case of internal or external shunts, treatment is to close the shunt surgically. Unfortunately, there is no way to close microscopic internal shunts. Therefore, treatment is aimed at decreasing toxins which are eliminated by the liver (ie decreasing protein ingestion).
Review videos
Dog abdominal vasculature – 28 min, watch until 35 min
Cat abdominal vasculature – 31 min
Key Terms
| Term | Notes (All structures exclusively found in the carnivore in this lab) |
| Cranial abdominal a. | Supplies craniodorsal abdominal body wall |
| Cranial epigastric a. | Supplies cranioventral abdominal body wall |
| Cranial superficial epigastric a. | |
| Deep circumflex iliac a. | Supplies caudodorsal abdominal body wall |
| Caudal epigastric a. | Supplies caudoventral abdominal body wall |
| Lumbar aa. | |
| Celiac a. | |
| Left gastric a. | |
| Hepatic a. | |
| Hepatic brr. | |
| Right gastric a. | |
| Gastrodoudenal a. | |
| Cranial pancreaticoduodenal a. | |
| Right gastroepiploic a. | |
| Splenic a. | |
| Short gastric aa. | |
| Left gastroepiploic a. | |
| Cranial mesenteric a. | |
| Middle colic a. | |
| Right colic a. | |
| Ileocolic a. | |
| Colic br. of ileocolic a. | |
| Cecal a. | |
| Mesenteric ileal a. | |
| Antimesenteric ileal a. | |
| Caudal pancreaticoduodenal a. | |
| Jejunal aa. | |
| Ileal aa. | |
| Phrenicoabdominal a./v. | |
| Adrenal gland | Be able to identify adrenal gland in situ. |
| Renal aa. | |
| Ovarian aa. | Female only |
| Testicular aa. | Male only; courses caudally through deep inguinal ring |
| Caudal mesenteric a. | |
| Left colic a. | |
| Cranial rectal a. | |
| (Hepatic) Portal vein |