Lab 2A: Urinary Bladder, pelvic urethra, pelvic and perineal muscles, and start comparative male genitalia
Learning Outcomes
- Identify the structures of the urinary bladder and pelvic urethra in males of the domestic species and compare and contrast this anatomy with the female anatomy.
- Identify the muscles of the urinary bladder and pelvic urethra; name their function and innervation and the type of innervation each nerve supplies.
- Identify the muscles associated with the anus and pelvic diaphragm.
The Urinary Bladder and Pelvic Urethra
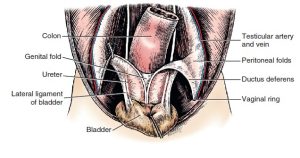
The urinary bladder is a muscular, expandable sac in the lower abdomen that serves as a temporary storage space for urine produced by the kidneys. The urinary bladder has an apex, a body, and a neck. Three connecting peritoneal folds (ligaments) are reflected from the bladder on the pelvic and abdominal walls. The median ligament of the bladder leaves the ventral surface of the bladder and attaches to the abdominal wall as far cranial as the umbilicus. In the fetus it contains the urachus and umbilical arteries. These degenerate and leave no ligamentous remnant in the adult. The lateral ligaments of the bladder pass from the left and right sides of the bladder to the pelvic wall and often contain an accumulation of fat along with the ureter and umbilical arteries (in the fetus, or if still patent in the adult). The round ligaments of the bladder, along the cranial free edges of the lateral ligaments of the bladder, are the adult remnants of the fetal umbilical arteries once they are no longer patent. All of the structures of fetal circulation will be covered in the lab over placentas.
-
Urogenital ligaments of the male, ventral
aspect. 1
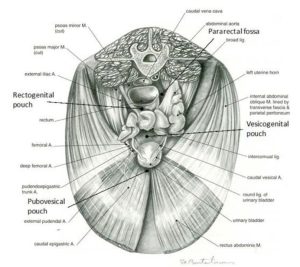
- Female goat pelvic viscera at pelvic inlet. 22
- Pelvic peritoneal pouches in a female (above) and male (below) animal. 7
Bundles of smooth muscle on the surface of the bladder pass obliquely across the neck of the bladder and the origin of the urethra. These bundles, collectively called the detrusor m., are innervated by the pelvic nerve (sacral parasympathetic neurons).
Recall that the ureters lie opposite each other near the neck of the urinary bladder. The trigone of the bladder is the dorsal triangular area located within the line drawn between the two ureteral openings and the lines connecting each ureteral opening with the urethral exit from the bladder.
No gross anatomical sphincter is present in the neck of the bladder, but a physiological sphincter of smooth muscle is innervated by the hypogastric nerves, which supply sympathetic visceral efferent innervation. This smooth muscle is called the internal urethral sphincter and is continuous with the detrusor muscle. It’s responsible for the involuntary control of urine flow from the bladder through the internal urethral orifice, which is the opening between the urinary bladder and pelvic urethra.
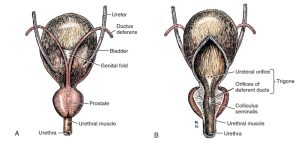
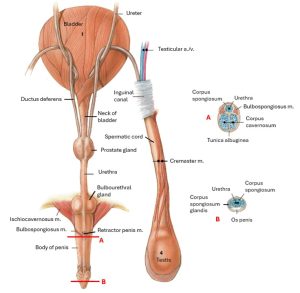
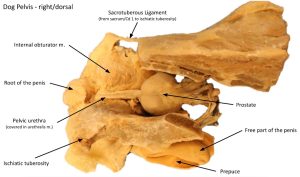
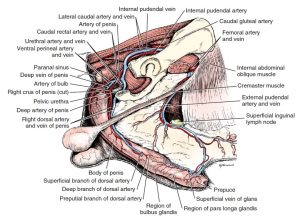
The male urethra is composed of a pelvic part (pelvic urethra) within the pelvis and a penile part within the penis (penile urethra). The prostate gland, a male accessory sex gland that contributes to the production of semen, completely surrounds the neck of the bladder and the beginning of the pelvic urethra. The subsection of pelvic urethra which passes through the prostate gland, which will be identified later, in males is sometimes called the prostatic urethra. Females, lacking both a penis and prostate gland, possess only a pelvic urethra.
FYI – Not far into the pelvic urethra there is a ridge of tissue projecting from the dorsal wall, the colliculus seminalis. Ejaculatory ducts have openings on this ridge, and provide a common outflow duct for the ductus deferens and vesicular gland (in those animals which possess vesicular glands – carnivores do not). On the lateral sides of the colliculus seminalis, there are numerous openings of the prostatic ducts of the compact portion of the prostate (stallion, bull, boar).
- Bladder and prostate. A, Dorsal aspect. B, Ventral aspect, partially opened on midline. 1
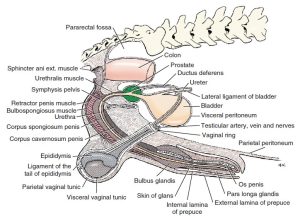
- Diagram of peritoneal reflections and the male genitalia. 1
- Male genital system of the cat with some muscles and prepuce removed, dorsal view. 4
- Male dog pelvic wall mm.
- Prostate gland of the dog
- Lateral contrast radiograph of the bladder and urethra in the male dog.
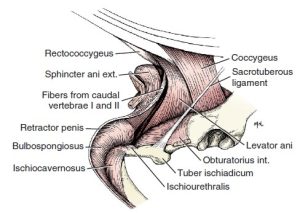
The urethral muscle (urethralis m) is striated and is confined to the pelvis, where it surrounds (in the male) the pelvic urethra and serves as a voluntary sphincter to retain the urine. In the female, the urethralis m. originates from the sides of the vagina and forms a sling ventral to the urethra and also serves as a voluntary sphincter. The pelvic urethra is continuous with the penile urethra in the male, which begins caudally at the level of the ischiatic crest, where the root of the penis is located. It DOES NOT extend around the penile urethra in the male. The urethralis muscle may also be called the external urethral sphincter. The urethralis m./external urethral sphincter is innervated by the pudendal nerve (sacral somatic efferent neurons).
Urine exits the urethra through the external urethral orifice. In the male, the external urethral orifice is located at the distal end of the penile urethra. The surrounding penile structures and their relationship with the penile urethra will be studied in depth during the dissection of the penis. The female animal, quite obviously, does not possess a penile urethra. In the female domestic species, the pelvic urethra empties into the vestibule through the external urethral orifice, which will be studied in relation to the female genitalia later in this unit.
Observe the pattern of the bundles of smooth muscle on the surface of the bladder (detrusor m). Identify the prostate gland in the male cadavers, a relatively large gland located just caudal to the neck of the bladder. Identify the pelvic urethra surrounded by (males), or supported by (females), the urethralis m.
Dissect: Make a ventral incision in the bladder wall (a cystotomy!) just to the left side of the medial ligament of the bladder, so as to keep the ligament intact. Extend the incision caudally towards the neck of the bladder, reaching the start of the urethra. In males, where possible, extend this incision through the prostatic urethra (a subpart of the pelvic urethra which runs through the prostate gland) and into the pelvic urethra. Come back to this last step later in the dissection if need be. Examine the mucosae of the bladder and urethra. If needed to better visualize these structures, you may transect the remaining abdominal wall. In doing so, avoid disrupting the superficial inguinal ring.
If the bladder is contracted, its mucosa will be thrown into numerous folds, or rugae, as a result of its inelasticity.
Observe the entrance of the ureters into the bladder and point to where the internal urethral sphincter (not a gross structure) is located – at the neck of the bladder, cranial to the prostate in the male and in an analogous position in the female. Identify the trigone of the bladder.
Observe: Review wet specimens with opened urinary bladder and incised pelvic urethra to study the urinary bladder and pelvic urethral anatomy of the ungulate species. Come back to this anatomy as you review the internal and external genitalia of the ungulate species.
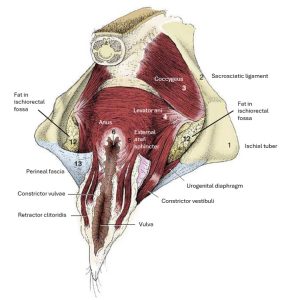
Perineum and Pelvic Diaphragm Muscles
The perineum is the region of the body superficial to the pelvic outlet. It extends ventrally from the base of the tail to the base of the scrotum in the male, and to below the vulva in the female. Laterally the perineum extends to the level of the ischiatic tuberosities. Its deep boundary is the pelvic outlet. Structures of the perineum include the anus, anal sphincter mm, the vulva in the female and the root of the penis in the male.
Observe: Take the time to observe the perineum of the cadavers in lab and note if they have normal confirmation or not.
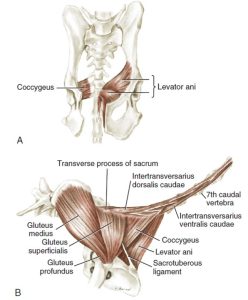
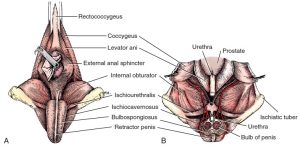
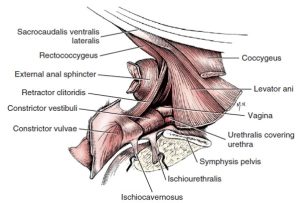
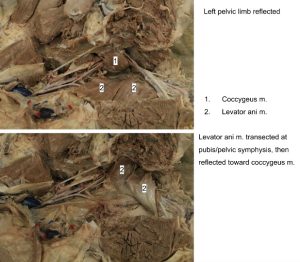
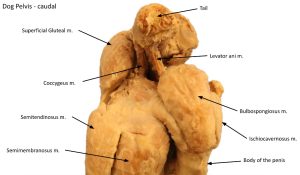
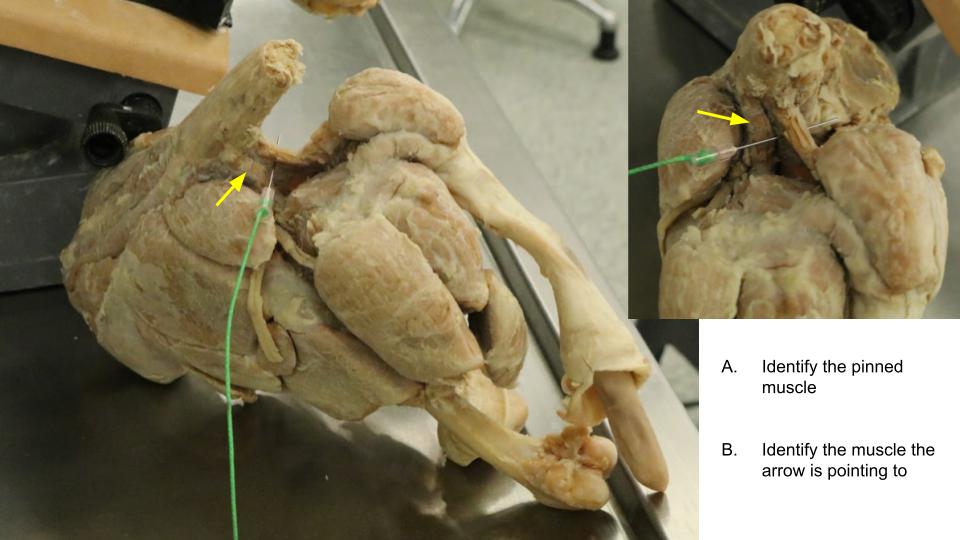
The levator ani and coccygeus muscles of each side form a pelvic diaphragm through which the genitourinary and digestive tracts open to the outside.
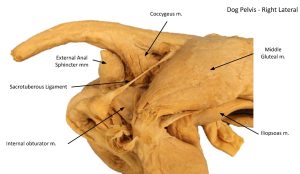
The levator ani muscle lies medial to the coccygeus muscle. It is a broad, thin muscle originating on the medial edge of the body of the ilium and the dorsal surface of the pubis and the pelvic symphysis. It covers the cranial part of the internal obturator. The muscle appears caudal to the coccygeus, where it inserts on caudal vertebrae 3 to 7. The coccygeus muscle lies lateral to the levator ani muscle. It is shorter and thicker and arises from the ischiatic spine and inserts on the transverse processes of caudal vertebrae 2 to 4. These muscles, in addition to the sacrotuberous ligament (in the dog) and the sacrosciatic ligament (in the ungulate), form the lateral soft-tissue boundaries of the pelvic cavity.
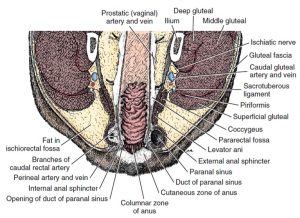
-
Muscles of the pelvis. A, Mm. levator ani and coccygeus, ventral
aspect. B, Caudal and gluteal muscles, lateral aspect. 1
- Anal region and root of the penis with superficial muscles, right lateral aspect. 1
- Perineal region of the male and female dog
- Male perineum. A, Superficial muscles, caudal aspect. B, Dorsal section through pelvic cavity. The bilobed bulb of the penis is transected, and the proximal portion removed. 1
- Constrictor muscles of female genitalia, lateral aspect. 1
- Perineal muscles of the cow. 8
Dissect: If not done when opening the pelvic cavity, transect the levator ani muscle at its pelvic attachments as close to dorsal pubis and pelvic symphysis as possible and then reflect it dorsally. The coccygeus m. likely does not need to be transected to visualize the vessels and nerves in close proximity (like internal pudendal a., pudendal n, and their branches, which you will be asked to locate later), but you may transect this muscle if necessary, especially in the dog. In the dog, these structures pass lateral to the pelvic diaphragm muscles. In the cat, these structures are located medial to the pelvic diaphragm mm and thus transection of these muscles may not be necessary.
- Male dog pelvic wall mm.
- Dog coccygeus and levator ani mm.
- Dog external anal sphincter
- Dog caudal view of pelvic wall mm.
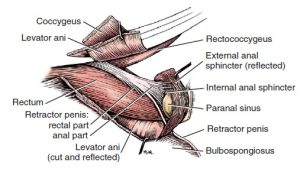
Recall that the the colon consists of the ascending, transverse, and descending colon. The rectum continues the descending colon through the pelvis. It begins at the pelvic inlet. The anal canal is a continuation of the rectum to the anus. Just inside the anus, at clock positions 8 and 4, respectively, you should find the openings to the paranal sinuses (anal sacs). The anal canal is surrounded by both a smooth internal anal sphincter muscle and a striated external anal sphincter muscle. The external opening of the anal canal is the anus.
- Muscles of the male anal region, lateral aspect. 1
- Topographic relations of the penis and other pelvic structures. 1
- Section through the anus of the dog in a dorsal plane. 1
The external anal sphincter muscle receives its nerve supply from the caudal rectal nerve (branch of the pudendal n.) and its blood supply from the caudal rectal a. (branch of the internal pudendal artery). The caudal rectal nerve provides voluntary control over defecation.
In the wall of the paranal sinus are microscopic glands, the secretion of which accumulates in the lumen. The secretion is held in the paranal sinus and is discharged through the duct of the paranal sinus into the anal canal during normal defecation. The microscopic glands are properly called the anal glands. In a clinical setting, it is sometimes necessary to manually express the paranal sinuses, which are often erroneously called the anal glands.
The internal anal sphincter muscle is an enlargement of the smooth circular muscle coat of the anal canal. It is not as distinct as the external anal sphincter.
The rectococcygeus muscle continues the longitudinal smooth muscle of the rectum to the ventral surface of the tail.
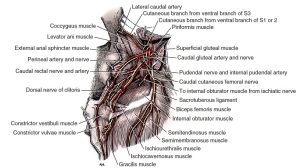
- Nerves, arteries, and muscles of the female perineum, caudolateral aspect. 1
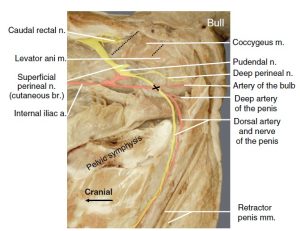
-
Sagittal section of the pelvis of a bull showing arterial supply of the penis. Note that the
internal pudendal artery and pudendal nerve make a cross (X) intersection close to the ischial arch. 12
- Constrictor muscles of female genitalia, lateral aspect. 1
Dissect: Transect the external anal sphincter muscle on the left and attempt to reflect it away from the underlying paranal sinus. The muscle is only a few millimeters thick and so transect carefully. If a full thickness incision is made into the paranal sinus, simply observe the external anal sphincter muscle on the outer surface of the paranal sinus. They need not be separated from each other at this point.
If not done already, now open the paranal sinus, expose its duct, and find the opening in the cutaneous zone of the anal canal. It may be possible to carefully insert a blunt probe through this duct. If possible, attempt to visualize the internal anal sphincter on your cadaver and/or observe it on a prosection, if available.
Longitudinally incise the skin a few centimeters on the left lateral surface of the tail base and reflect the skin dorsally and ventrally. Isolate the dorsal anal region and identify a pale band of muscle arising from the dorsal rectal wall cranial to the sphincter muscles, and extending caudally a few centimeters or so, to its insertion on the ventral midline of the tail. This is the rectococcygeus muscle.
Clinical Application: Perineal hernias
Perineal hernias are herniation of caudal abdominal contents between the muscle layers of the pelvic diaphragm and pelvic outlet. Weakening of these mm is associated with straining to defecate, such as occurs in intact males with benign prostatic hyperplasia. Herniation occurs most commonly between the levator ani m and the external anal sphincter m. Repair involves elevation of the internal obturator mm from the ischium to help close the defect. Structures to be identified and preserved are the pudendal n, caudal rectal n, and internal pudendal a/v. Castration of intact males is done in conjunction with surgical repair of the hernia. Be certain not to disrupt the caudal rectal nerve, damage to which can cause irreversible fecal incontinence.
Clinical Application: Paranal Sinus Impaction/Infection
Clinical signs of an animal whose anal sacs are not draining are persistent licking at the perineal region, a distinctive smell (you just have to smell it if you haven’t already), and “scooting” the perineum along the ground or carpet. Preferred digital expression of the anal sacs requires entering the anal canal with the pointer finger, reaching cranial to the anal sac, and the thumb on the lateral aspect of the animal to gently “milk” the secretions out through the anal sac duct. If too much resistance occurs in doing so, stop before rupture of the anal sac occurs. Always express both sides.
If impacted anal sacs are left untreated, an abscess may occur, necessitating lancing of the sac followed by antimicrobial and pain therapy. If regularly expressing the paranal sinuses fails to prevent recurrence of anal sac infection, an anal saculectomy may be indicated.
- Expression of the left anal sac
- Infected and abscessed right anal sac.
- Anal sacculectomy
Review videos
Pelvic wall muscles – watch until 4 min
Dog bladder and pelvic urethra – 5 min, watch until 6:30
Terms
| Urinary Bladder | ||
| Term | Features | Species differences/comments |
| Urinary bladder | Apex | |
| Neck | ||
| Trigone | Know boundaries | |
| Ligaments of the bladder | Median | Only one median ligament of the bladder. |
| Lateral | ||
| Round | Cranial free edges of the lateral ligaments. | |
| Ureters | Spelling counts here. Do not confuse with urethra! | |
| Ureteral openings | ||
| Detrusor m. | On surface of bladder but viewable grossly | |
| Internal urethral sphincter | Smooth muscle surrounding internal urethral orifice | |
| Internal urethral orifice | ||
| Urethra | ||
| Term | Features | Species differences/comments |
| Pelvic urethra | ||
| Prostatic urethra | ||
| Penile urethra | ||
| Urethralis m./external urethral sphincter | ||
| External urethral orifice | Female – empties into the vestibule
Males – empties at the distal end of the penis |
|
| Perineum and Pelvic Diaphragm Muscles | ||
| Term | Features | Species differences/comments |
| Levator ani m. | ||
| Coccygeus m. | ||
| Rectum | ||
| Anus | ||
| Anal canal | Continuation of the rectum to the anus | |
| Paranal sinuses (anal sacs) | ||
| Internal anal sphincter muscle | ||
| External anal sphincter muscle | ||
| Caudal rectal nerve | Provides voluntary control over defecation | Innervates external anal sphincter. Do not ID at this juncture. Know conceptually. |
| Rectococcygeus muscle | ||